The Magnitude of Obesity and its Relationship to Blood Pressure Among the Residents of Enugu Metropolis in South East Nigeria
- *Corresponding Author:
- Dr. Okafor CI
Department of Medicine, College of Medicine, University of Nigeria, Enugu Campus, Enugu, Nigeria.
E-mail: christian.okafor@unn.edu.ng
Abstract
Background: Obesity in developing nations is no longer as uncommon as it was thought to be decades ago however paucity of data on the burden of obesity from urban communities was observed by previous workers. Aim: To determine the magnitude of obesity and its relationship to blood pressure among urban adult residents in Enugu metropolis. Subjects and Methods: A cross‑sectional community survey of adults who were not known to have diabetes or hypertension by self‑report was carried out. Four parts of the metropolis selected by simple random sampling were used and consenting individuals aged 18‑70 years were consecutively recruited. Anthropometric measurements were done using standard procedures as specified in the World Health Organization STEPs instrument. Obesity was determined using widely acknowledged body mass index (BMI) ≥30 kg/m2. Descriptive and inferential statistical analyses was performed using SPSS with P value set at < 0.05. Results: A high prevalence of obesity of 21.2% (95% confidence interval [CI]: 18.3‑24.1) was found among the participants with significant female gender preponderance. The burden increased with age with the middle age group highly involved. Attainment of age of 40 years and above had an increased odd of developing obesity (odds ratio = 1.8; 95 % CI: 1.3‑2.6). There was a relationship between blood pressure and BMI as shown by positive correlation, higher BMI among hypertensive subjects and high burden of elevated blood pressure among obese subjects (91/164; 55.5%). Conclusion: A high magnitude of obesity existed among this apparently healthy unaware adults resident in an urban Nigerian city and obesity is associated with elevation in blood pressure.
Keywords
Blood pressure, Nigeria, Obesity, Urban residents
Introduction
The excess accumulation of body fat widely known as obesity is associated with several chronic non-communicable diseases such as diabetes, hypertension, cancers, respiratory tract disorders, and osteoarthritis. Globally in 1997, obesity was formally recognized by World Health Organization (WHO) as an epidemic disorder; a phenomenon that is now common to both developed and developing nations.[1] Physiologically, while recognizing some influence from the genetic makeup of the individual, weight gain is primarily a function of energy intake and expenditure. In the developing nations, the increase in the burden of obesity was initially noted among the higher socioeconomic strata, but currently, the trend is now shifting towards the lower socioeconomic strata.[2] The key driving forces toward obesity are urbanization and globalization of food production and marketing.[3] In the developing nations, the change in lifestyle of the urban dwellers is characterized by some form of improved earnings, increased technological advancement, which leads to reduced physical activity level and increased intake of calorie-laden diets, which are common with many fast food centers.
Data on the burden of obesity from Africa is beginning to emerge and recent systematic reviews of publications on obesity show that obesity is no longer as uncommon as it was several decades ago.[4,5] The WHO consultative committee according to Caballero[2] observed then that data on the magnitude of obesity was unavailable for Sub-Saharan Africa except for Mauritus and South Africa. Prevalence rates of obesity determined using body mass index (BMI) as reported by several Nigerian authors working among diverse populations ranges from 4.2% (low) to 49% (high).[6-11]
The cardiometabolic consequences of obesity are strongly related to endothelial dysfunction.[12] Therefore, a rise in the burden of obesity as is the current trend could also lead to a rise in the burden of cardiometabolic disorders such as diabetes and hypertension. Subjects without diabetes and hypertension may consider themselves to be healthy being unaware of their cardiometabolic risk and its likely consequences due from their overweight or obese status. This study aimed at determining the magnitude of obesity and its relationship to blood pressure among urban residents in Enugu metropolis using adult individuals with self-reported absence or unawareness of diabetes or hypertension. Being a community survey and being not aware of any similar community-based study in purely urban dwellers, the study aimed at determining the burden of obesity and its relationship among urban residents of the metropolis. This study will also help bridge the gap or paucity of community-based data on noncommunicable diseases from this part of the country as acknowledged by other authors who have studied rural and semi-urban populations in the same area.[13,14]
Subjects and Methods
Adult subjects (18-70 years) resident in Enugu metropolis who are of the Ibo tribe, resident in the metropolis for at least a year, and had no history of hypertension or diabetes by self-report were recruited for this cross-sectional study from four out of eight parts of the metropolis (namely Abakpa, Trans-Ekulu, Emene and Asata) which were selected by simple random sampling. Recruitment was conducted from June 2006 to March 2007. Enugu is the current capital city of Enugu State. It is inhabited by people, which cut across diverse occupational groups such as civil servants, traders, industrialists, artisans, farmers etc. Its population according the 2006 population census is 722,664.[15]
Using a table for determination of sample size[16] the minimum sample size needed for this study which corresponds to expected sample sizes when studying a population of 1 million and above was 384 subjects. This also corresponded with the figure obtained when sample size determination is done using the formula:
N=z2 pq / d2
when studying proportions with population >10,000 individuals[17] (where n is the desired sample size required for valid result, z = standard normal deviate set at 1.96 which corresponds to the 95% confidence level., P = proportion of target population estimated to have the outcome measure (obesity) and where no reasonable estimate exists 50% (0.5) is advised to be used. A total of 792 participants were consecutively recruited having aimed at 200 participants from each part. Consent was duly obtained from the subjects and those at risk were further counseled individually. The subjects were invited for the study after some health awareness campaigns and education on common noncommunicable diseases (hypertension and diabetes) were delivered to the subjects who participated in medical mission outreaches conducted on different days in these communities. Participants were not however limited to people residing in those four parts of the metropolis. A total of 775 subjects were subsequently used for analyses after data cleaning. Clinical data collection (by interviewer-administered questionnaire) and measurements were carried out as provided in the WHO STEPS instrument on surveillance of behavioral risk factors (version 2).[18] Obesity and hypertension as the primary outcome measures were determined using BMI of ≥30 kg/m2 and systolic and/or diastolic pressure of ≥140 mm Hg and ≥90 mm Hg respectively. Subjects’ weights were measured with a weighing balance while their heights were measured with a wall mounted stadiometer. Different examination rooms were dedicated to males and females respectively for privacy. Measurement of waist circumference was done with subjects in light clothing. Waist circumference was measured midway between the angle of the ribs and the iliac crest, while hip circumference was measured at the level of the greater trochanters. Their blood pressures were also measured using digital sphygmomanometers (Omron® HEM-712C, China), which were always calibrated using mercury sphygmomanometers on each day of data collection. Measurements were taken with each subject sitting down. Average of second and third readings was used to determine each participant’s blood pressure.
Ethical clearance was obtained from the Health Research and Ethics Committee of University of Nigeria Teaching Hospital, Enugu. Data entry and analysis were performed with IBM SPSS 20 (released 2011; IBM Corp. Amonk, NY) with level of significance set at P < 0.05. T-test and Analysis of Variance (ANOVA) were used for comparison of means while Chi-square and Pearson’s correlation were used for test of association and correlation respectively.
Results
A total of 775 participants (279 males and 496 females) giving a male: female ratio of 1:1.7 were used for data analysis. The clinical characteristics in Table 1 show some significant differences between male and female participants. The male participants were older, taller and heavier than the female participants. Among the indices of obesity, only BMI and waist circumference showed significantly higher mean values among the females. Using ANOVA, clinical characteristics except age showed a significantly clear increase in mean values as BMI status increased among the participants [Table 2].
| Clinical characteristic | Mean (SD) | P value* | |||||
|---|---|---|---|---|---|---|---|
| Males (n=279) | Females (n=496) | All (n=775) | |||||
| Age (years) | 50.8 | (13.7) | 48.2 | (12.5) | 49.1 (13) | <0.01 | |
| Height (m) | 1.7 | (0.1) | 1.6 | (0.1) | 1.7 | (0.1) | <0.001 |
| Weight (kg) | 73.6 (12) | 70.7 | (12.4) | 71.7 | (12.3) | <0.01 | |
| WC (cm) | 90.1 | (10.6) | 92.1 | (11.7) | 91.4 | (11.4) | 0.02 |
| HC (cm) | 96 (8.9) | 100.6 (10.1) | 98.9 (9.9) | <0.001 | |||
| SBP (mmHg) | 133.5 (23.9) | 134.9 (23.4) | 134.4 (23.6) | 0.40 | |||
| DBP (mmHg) | 83.4 (14) | 81.8 | (13.3) | 82.4 | (13.6) | 0.09 | |
| BMI (kg/m2) | 25.4 (3.8) | 26.9 (4.4) | 26.4 (4.2) | <0.001 | |||
| WHR | 0.94 | (0.07) | 0.92 | (0.08) | 0.92 | (0.07) | <0.001 |
*Level of significance between males and females. SD: Standard deviation, BMI: Body mass index, WHR: Waist hip ratio, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, WC: Waist circumference, HC: Hip circumference
Table 1: Clinical characteristics of the male and female subjects
| Clinical characteristic | Mean (SD) | ANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI groups (kg/m2) | F (4, 770) | P value | ||||||
| <18.5 | 18.5-24.9 | 25-29.9 | 30-34.9 | 35-39.9 | ||||
| Age (years) | 52.3 (10.5) | 47.7 (15) | 50 (11.7) | 49.6 (10.5) | 52.8 (9.9) | 2.0 | 0.09 | |
| Height (m) | 1.67 (0.08) | 1.66 (0.09) | 1.65 (0.08) | 1.64 (0.06) | 1.6 (0.08) | 3.8 | <0.01 | |
| Weight (kg) | 50.8 | (3.5) | 61.6 (7.7) | 74.2 (7.1) | 85.6 (6.7) | 93.7 (10.6) | 343.8 | <0.001 |
| WC (cm) | 73.8 | (5.5) | 82.9 (8.6) | 93.9 (8.0) | 102.2 (6.5) | 108.2 (9.3) | 189.9 | <0.001 |
| HC (cm) | 90.5 | (1.0) | 91.2 (7.0) | 100.9 (7.7) | 108.2 (7.3) | 114.8 (4.4) | 175.8 | <0.001 |
| SBP (mmHg) | 103.2 (4.5) | 131.8 (23.4) | 136.9 (23.1) | 135 (24) | 138.6 (25.1) | 3.8 | <0.01 | |
| DBP (mmHg) | 73 | (2) | 80.8 (12.3) | 81.6 (13.2) | 87.7 (16.6) | 83.3 (8.1) | 7.2 | <0.001 |
| BMI (kg/m2) | 18.2 | (0.5) | 22.4 (1.6) | 27.3 (1.4) | 31.7 (1.3) | 36.4 (1.2) | 1442 | <0.001 |
| WHR | 0.81 (0.05) | 0.91 (0.08) | 0.93 (0.07) | 0.95 (0.06) | 0.94 (0.07) | 13.4 | <0.001 | |
WC: Waist circumference, HC: Hip circumference, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, BMI: Body mass index, WHR: Waist hip ratio, SD: Standard deviation
Table 2: Clinical characteristics by categories of BMI for all subjects (n=775)
Prevalence of obesity
Among the participants, 164 out of 775 were obese. Hence the prevalence of obesity was 21.2 % (164/775) (95% confidence interval [CI]: 18.3-24.1). One hundred and twenty female subjects out of 496 (24.2%) had obesity compared to 44/279 (15.8%) male participants thus showing obesity to be more prevalent among the female participants (P < 0.01). Overweight was seen in 295 participants giving a prevalence of 38.1% (95% CI: 34.6-41.6). Overweight was equally more common in females (40.1%; 199/496) than males (34.4%; 96/279). Underweight was seen in only 0.5% (4/775) of participants.
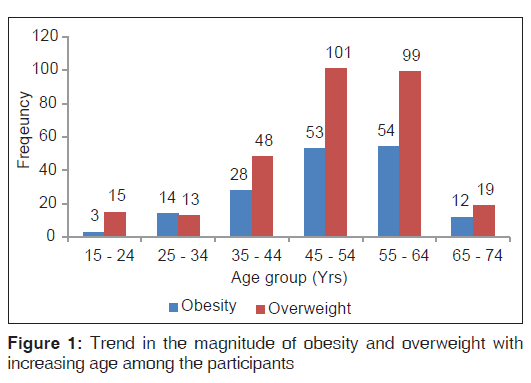
Obesity and overweight increased with age among the participants with greater involvement of middle age bracket [Figure 1]. This age-related trend was common to both genders. Age was significantly associated with overweight or obesity (P < 0.01); the odd of overweight or obesity was significantly increased with attainment of ≥40 years of age (odds ratio = 1.8; 95% CI: 1.3-2.6).
Relationship between blood pressure and obesity
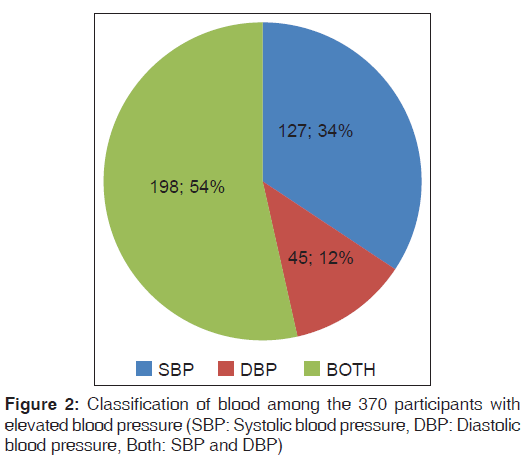
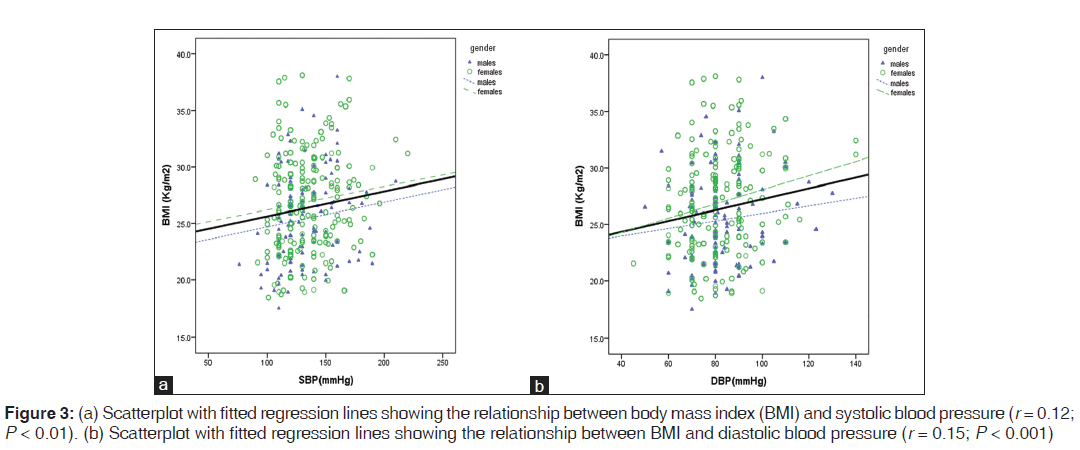
Among all the 775 participants, elevated blood pressure was observed in 370 (47.7%; 95% CI: 44.1-51.3) participants. Majority of these 370 subjects had both elevated systolic and diastolic blood pressure as shown in [Figure 2]. Systolic and diastolic blood pressures were positively but weakly correlated with BMI [Figure 3a and b]. Participants observed to have elevated blood pressure were noted to have higher BMI (26.8 vs. 25.9 kg/m2; P < 0.01). Furthermore, across the BMI groups [Table 2], systolic blood pressure and diastolic blood pressure significantly increased as BMI group increased (P < 0.01 and < 0.001 respectively). More than half (91/164; 55.5%) of the obese persons had elevated blood pressure. This association was significant (P = 0.03). The odd for developing high blood pressure in the presence of obesity was 1.5 (95% CI: 1.1-2.1). Relatively, over 50% of male (52.3% [23/44]) and female (56.7% [68/120]) obese subjects had elevated blood pressure.
Discussion
This study which sought to evaluate the real community burden of excess weight among the residents of an urban city in Nigeria demonstrated a high magnitude of overweight and obesity among these apparently healthy participants. In other words, a lot of urban residents may be unaware of their health risk burden. A high prevalence of obesity of 21.2% will tend to suggest that about one in every five urban dweller is obese using a well-recognized WHO standard for classification. Similarly, higher burden of persons in the overweight category was also observed. This trend when compared to some earlier reports by Bakari and Onyemelukwe[7] and Puepet et al.[6] goes along the recently observed global trend of increasing prevalence of obesity especially among urban dwellers.[2] The obesity epidemic has been attributed to the “obesogenic” environment being created as a result of reduced physical activity and increased availability and consumption of calorie-dense foods all of which are characteristics of many urbanized nations.[1,3] The physiologic effect of this demographic transition is simply a reduction in energy expenditure against excess energy intake. Several other reasons such as genetic predisposition, rural-urban drift and socioeconomic positions are implicated as contributory factors too.[19,20] The impact of urban residence in similar population as ours has also been observed by others authors.[21,22] Though the association between obesity and urbanization has been widely acknowledged, Voss et al.[23] found an inverse association between obesity prevalence and urbanization. This was probably thought to be due to the effect of elevation or altitude on several physiologic mechanisms such as hypoxia, leptin signaling, metabolic demands and norepinephrine levels.
Adienbo et al.[11], found a much higher prevalence of about 47% in another Nigerian ethnic group of Niger Delta region where the influence of certain cultural practices (fattening room experience) peculiar to women was found to significantly contribute to higher burden of obesity among the women. The burden of overweight and obesity was demonstrated in this study to be higher among the females. They also had higher mean BMI. This trend of gender involvement has been observed in several studies dating back to about three decades ago.[11,24,25] Hormonal influences, cultural practices, and less energy demanding occupational engagements may be additional contributory factors to genetic differences, which may account for the female gender preponderance.[11,26,27]
As reported by other workers, the magnitude of obesity was found to increase with advancing age with peak among those in their late thirties to forties.[9,28] Attainment of 40 years of age had increased significant odds of developing obesity. This peak age involvement in recent studies tends to move toward involvement of younger people when compared to the 55-64 year age group reported by Johnson in the seventies.[24] This may not be unconnected to the decreasing level of physical activity among the youths who appear to be caught most by the current wave of technological advancements.[29] They younger age groups are also the age groups mostly involved in rural-urban drift not only in pursuit of better jobs but also due to availability of attractive social amenities in the urban cities. Thus leaving the elderly people to retire to the rural villages may result in the reduction of the burden of obesity among the elderly as found in this study. The involvement of young age and the productive age groups again could have untoward consequences as the nation’s economy may be greatly affected by decreased or loss of productivity. The increase in burden of obesity over time could result in increased burden of other noncommunicable cardiometabolic diseases, which could also lead to attendant loss in productivity as a result of loss of man-hours and high cost of health care maintenance.
This study found a significant correlation and association between obesity and blood pressure; both in the linear relationship between absolute values and association in terms of proportion of individuals affected. Obesity has been described as one of the novel risk factors for endothelial dysfunction, and it is linked to cardiovascular diseases such as hypertension and diabetes.[12] Thus, endothelial dysfunction as observed in obese individuals causing arterial wall proliferation and impaired vasomotor tone could be the link between obesity and elevated blood pressure.[30] Several other mechanisms such as abnormality in pressure natriuresis, hyperinsulinemia and insulin resistance, activation of the renin angiotensin system and involvement of the sympathetic nervous system have been implicated in obesity-induced elevation of blood pressure.[31]
It is to be remarked that the cross-sectional design of this study, which weakens the likelihood of any causal relationship is a limitation to be noted in interpretation of findings of this investigation. Secondly, other metabolic parameters such as fasting blood glucose and total fasting cholesterol, which would have further characterized these subjects, were not measured in this study to avoid exposing some of the participants who were assessed later in the day to prolonged fast.
Conclusion
This study showed a high magnitude of overweight and obesity among an urban adult population in south east Nigeria; a finding that is supportive of the growing obesity epidemic in developing nations. Obesity was also seen to be associated with a high burden of hypertension among this group of people who were considered to be apparently healthy or without hypertension and/or diabetes.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. Geneva, Switzerland: World Health Organization; 2000. [WHO Technical Report Series 894].
- Caballero B. The global epidemic of obesity: An overview. Epidemiol Rev 2007;29:1-5.
- Hoffman DJ. Obesity in developing countries: Causes and implications. Food Nutr Agric 2001;28:35-44.
- Adeboye B, Bermano G, Rolland C. Obesity and its health impact in Africa: A systematic review. Cardiovasc J Afr 2012;23:512-21.
- Chukwuonye II, Chuku A, John C, Ohagwu KA, Imoh ME, Isa SE, et al. Prevalence of overweight and obesity in adult Nigerians – A systematic review. Diabetes Metab Syndr Obes 2013;6:43-7.
- Puepet FH, Zoakah AI, Chuhwak EK. Prevalence of overweight and obesity among urban Nigeria adults in Jos. Highland Med Res J 2002;1:13-6.
- Bakari AG, Onyemelukwe GC. Indices of obesity among type 2 diabetic Hausa-Fulani Nigerians. Int J Diabetes Metab 2005;13:28-9.
- Ulasi II, Ijoma CK, Onodugo OD, Arodiwe EB, Ifebunandu NA, Okoye JU. Towards prevention of chronic kidney disease in Nigeria: A community-based survey in southeast Nigeria. Kidney Int suppl 2013;3:195-201.
- Gezawa ID, Puepet FH, Mubi BM, Uloko AE, Bakki B, Talle MA, et al. Prevalence of overweight and obesity in Maiduguri, North-Eastern Nigeria. Niger J Med 2013;22:171-4.
- Onyechi UA, Okolo AC. Prevalence of obesity among undergraduate students living in halls of residence, University of Nigeria Nsukka Campus. Anim Res Int 2008;5:928-31.
- Adienbo OM, Hart VO, Oyeyemi WA. High prevalence of obesity among indigenous residents of a Nigerian ethnic group: The Kalabaris in the Niger delta region of South South Nigeria. Greener J Med Sci 2012;2:152-6.
- Caballero AE. Endothelial dysfunction in obesity and insulin resistance: A road to diabetes and heart disease. Obes Res 2003;11:1278-89.
- Ahaneku GI, Osuji CU, Anisiuba BC, Ikeh VO, Oguejiofor OC, Ahaneku JE. Evaluation of blood pressure and indices of obesity in a typical rural community in eastern Nigeria. Ann Afr Med 2011;10:120-6.
- Ulasi II, Ijoma CK, Onodugo OD. A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res 2010;10:71.
- Legal Notice on Publication of the Details of the Breakdown of the National and State Provisional Totals 2006 Census. Vol. 94. No. 24. Lagos: Official Gazette, Federal Republic of Nigeria; 2007. p. B 175-98.
- Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas 1970;30:607-10.
- Araoye MO. Research Methodology and Statistics for Health and Social Sciences. Ilorin: Nathadex Publishers; 2003. p. 115-29.
- World Health Organization. WHO STEPwise approach to chronic disease risk factor surveillance- Instrument v2.0. Department of Chronic Diseases and Health Promotion. World Health Organization. 20 Avenue Appia, 1211 Geneva 27, Switzerland. (Available at http://www.who.int/chp/ steps). [Accessed on 2006 Mar 31].
- Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, et al. The effect of rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS Med 2010;7:e1000268.
- Sovio U, Giambartolomei C, Kinra S, Bowen L, Dudbridge F, Nitsch D, et al. Early and current socio-economic position and cardiometabolic risk factors in the Indian Migration Study. Eur J Prev Cardiol 2013;20:844-53.
- Ekezie J, Anyanwu EG, Danborno B, Anthony U. Impact of urbanization on obesity, anthropometric profile and blood pressure in the Igbos of Nigeria. N Am J Med Sci 2011;3:242-6.
- Ejim EC, Onwubere BJ, Okafor CI, Ulasi II, Emehel A, Onyia U, et al. Cardiovascular risk factors in middle-aged and elderly residents in South-East Nigeria: The influence of urbanization. Niger J Med 2013;22:286-91.
- Voss JD, Masuoka P, Webber BJ, Scher AI, Atkinson RL. Association of elevation, urbanization and ambient temperature with obesity prevalence in the United States. Int J Obes (Lond) 2013;37:1407-12.
- Johnson TO. Prevalence of overweight and obesity among adult subjects of an urban African population sample. Br J Prev Soc Med 1970;24:105-9.
- Desalu OO, Salami AK, Oluboyo PO, Olarinoye JK. Prevalence and socio-demographic determinants of obesity among adults in an urban Nigerian population. Sahel Med J 2008;11:61-4.
- Ngwu EK. Prevalence of obesity and some of its complications among high risk individuals in Enugu metropolis. West Afr J Foods Nutr 2007;8:9-16.
- Lovejoy JC. The influence of sex hormones on obesity across the female life span. J Womens Health 1998;7:1247-56.
- Yusuf SM, Mijinyawa MS, Musa BM, Gezawa ID, Uloko AE. Overweight and obesity among adolescents in Kano, Nigeria. J Metab Syndr 2013;2:126.
- Vandelanotte C, Sugiyama T, Gardiner P, Owen N. Associations of leisure-time internet and computer use with overweight and obesity, physical activity and sedentary behaviors: Cross-sectional study. J Med Internet Res 2009;11:e28.
- Widlansky ME, Gokce N, Keaney JF Jr, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol 2003;42:149-60.
- Hall JE. Louis K. Dahl Memorial Lecture. Renal and cardiovascular mechanisms of hypertension in obesity. Hypertension 1994;23:381-94.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.