The Millennium Development Goal 6 Partnership for African Clinical Training (M-PACT) Clinical Course: A Six Months’ Post Training Impact Survey
2 Royal College of Physicians of London, 11 St Andrews Place, Regent’s Park, NW1 4LE London, UK, Email: kathryn345@gmail.com
3 Hepatology Unit, Imperial College London, 10th Floor, QEQM Building, St Mary’s Hospital Campus, South Wharf Road, W2 1NY, London, UK, Email: jin123@gmail.com
4 West African College of Physicians (WACP), 6 Taylor Drive, Off Edmond Crescent, Yaba Lagos Nigeria/Department of Medicine, College of Medicine, University of Ibadan/University College Hospital Ibadan, Oyo State, Nigeria, Email: babatunde123@gmail.com
5 West African College of Physicians (WACP), 6 Taylor Drive, Off Edmond Crescent, Yaba Lagos Nigeria/Korle Bu Teaching Hospital, Accra, Ghana, Email: albert123@gmail.com
6 West African College of Physicians (WACP), 6 Taylor Drive, Off Edmond Crescent, Yaba Lagos Nigeria/ Université de Thiès, Région de Thiès, Sénégal, Ghana, Email: mourtalla123@gmail.com
Citation: Jin Un Kim. The Millennium Development Goal 6 Partnership for African Clinical Training (M-PACT) Clinical Course: A Six months’ Post Training Impact Survey. Ann Med Health Sci Res. 2017; 7:284-288
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Context: The Royal College of Physicians of London and the West African College of Physicians have a long history of collaboration with a focus on postgraduate education. The Millennium Development Goal 6 Partnership for African Clinical Training (M-PACT) Clinical Course project was undertaken to improve the theoretical and practical knowledge base in the pertinent diseases of the Millennium Developments Goals (MDG 6): Tuberculosis, HIV/AIDS, Malaria, and medical leadership. Aim: To assess the impact of the training on everyday practice of the participants at least six months’ post training. Material and methods: A cross-sectional descriptive survey was used to execute this study between April to May 2016. A self-administered questionnaire was used for this study. Questionnaires were distributed using SurveyMonkey®. Data were analyzed using SurveyMonkey® Analysis Tool and Microsoft Excel Sheet. Results: A total of 73 trainees from six different courses responded to the survey. Majority (76.06%) of all respondents were from tertiary facilities. The survey revealed a positive influence on the clinical practice of participants, on prescription patterns, diagnostic approaches, and case findings in the community. A number of new concepts such as “Doctors as Leaders” were learned by the participants with over 80% of respondents desiring further trainings in leadership. Conclusion: The M-PACT courses had changed the knowledge base of the participants with more confident diagnosis, management and prescribing reported as a result. We suggest that this format for postgraduate teaching is important not only in West Africa, but throughout sub-Saharan Africa.
Keywords
Clinical Training; West Africa; Royal College of Physicians; West African College of Physicians; M-PACT
Introduction
In the West African sub-region, communicable diseases such as Malaria, Tuberculosis and HIV have remained a major cause of morbidity and mortality resulting in poor health outcomes [1,2]. The recent Ebola Viral Disease outbreak in the region devastated the health system, killed scarce healthcare workers and reversed the healthcare gains in the region [3-6]. Building and improving on the skill sets of technical healthcare workers is critical towards the achievement of the various world development goals. In-service training of healthcare workers has, over the years, been shown to improve health outcomes including impacting positively on the availability and quality of Emergency Obstetrics Care with “up-skilling” of midwives [7]. Human resources for health is a critical issue in Sub-Saharan Africa as the decision to enter, remain and work in the health sector workforce is influenced by several factors, including the use of monetary and non-monetary incentives to have the accurate skill mix in the appropriate place [8].
Achieving the Millennium Development Goals (MDGs) and Sustainable Development Goals (SDGs) in resource-poor settings will still require significant investment in continuous in-service training of relevant healthcare workers. This is critical, as training of healthcare workers has been shown to improve the quality and use of healthcare services [9].
To this end, the Royal College of Physicians of London (RCP) and the West African College of Physicians (WACP) have had several progressive, educationally-focused partnerships over the past decade. These have led to the training of hundreds of physicians in various aspects of clinical practice, development of curricula and strengthening of health systems. In 2013, the Royal College of Physicians partnered with the West African College of Physicians with funding from Ecobank Foundation (Lomé, Togo) to execute a 3-year clinical training for physicians in the West African Region. This partnership, named Millennium Development Goal 6 Partnership for African Clinical Training (M-PACT) was designed to conduct 15 clinical training courses on management aspects of Tuberculosis (TB), HIV and Malaria over a period of 3 years in four key West African countries- Nigeria (Abuja and Ibadan), Ghana (Accra), Sénégal (Dakar) and Sierra Leone (Freetown).
Participants were drawn from all the countries in the region. By the end of the second year, 10 clinical courses were conducted with participants drawn from 11 nations in four principal learning centers of Ibadan, Abuja, Accra and Dakar. These courses reached 294 physicians in the region. In addition, three “doctors as educators” training courses were also held in Abuja, Ibadan and Accra, reaching 101 consultants and trainers of medical doctors and students. Although a number of participants were in their residency training, most of the doctors who attended the courses had not previously had the opportunity of attending such formal and high quality training for some time.
The aim of this evaluation was to assess the impact of the first six courses in the practices and networking of trained physicians in their respective centers and communities.
The study was designed to answer the following research questions:
1. What is the effect/impact of the “MDG 6 Partnership for African Clinical Training” on the practice of trained physicians, participating in the programme?
2. What new concepts were acquired by the participants from the training?
3. How had the participants applied their new knowledge in day-to-day clinical and leadership roles in their different locations across West Africa?
Subjects and Methods
We used a cross-sectional descriptive approach for this study. We included all participants who participated in the M-PACT course 6 months prior to the evaluation. Six cohorts (two each from Nigeria, Ghana and Sénégal were included in this study).
Field work took place between April to May, 2016. A comprehensive database of all qualified trainees was developed and validated by the RCP/WACP M-PACT team in London and in Nigeria. A self-administered questionnaire was developed in both English and French, as participants on the course were drawn from both Francophone and Anglophone nations of West Africa.
Reverse translation was used to validate the questionnaire. We disseminated the questionnaire to selected trainees using the SurveyMonkey® Survey Tool (SMST – Palo Alto, California, USA) [10]. Participants were given a 2-week timeline to complete and return the completed questionnaire.
Participants were informed of the survey through three separate e-mails.
Participation in the survey was optional and consents were obtained from trainees during the training programme in Nigeria, Ghana and Sénégal in 2014 and 2015. Completed questionnaires received before the deadlines were collated and analyzed using the SMST analysis tool and MS Excel (Microsoft, Redmond, Washington, USA) [11]. Further analysis was performed using SPSS vs. 21 (IBM, Armonk, New York, USA).
Results
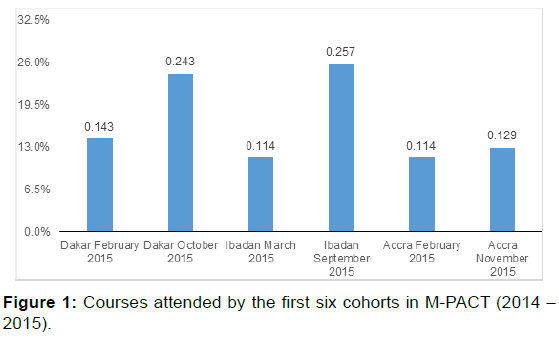
A total of 73 trainees out of 187 responded to the survey, giving a response rate of 39%. Participants were drawn from six different M-PACT courses as shown in Figure 1.
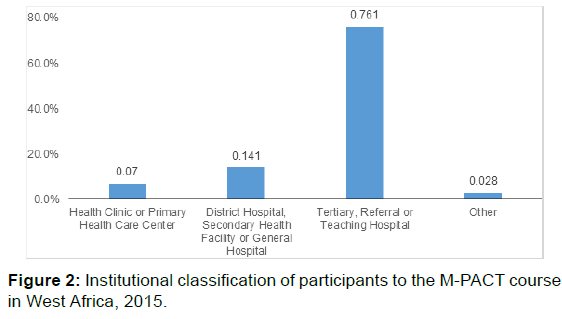
The survey showed that 14.29% and 24.29% of the respondents were drawn from the February and October 2014 courses in Dakar; 11.43% and 25.71% from the Ibadan September 2014 course and 11.43% and 12.86% from the Accra courses in February and November 2014. Of the 191 participants in the six courses, about 30 came from each course as shown in Table 1. 76.06% of all respondents were from tertiary facilities. The rest were from healthcare centers and other primary healthcare facilities (7.04%), district or secondary facilities (14.08%) and other forms of healthcare facilities including non-governmental organizations (2.82%) as shown in Figure 2. The training influenced various aspects of practice of the participants. Apart from the standard topics covered during the one-week course, participants also learnt a number of new concepts. These include “Doctors as Leaders” career development management concepts, new ideas on the control and treatment of HIV and TB including paediatric management, disease outbreak and infection prevention and the use of personal protective equipment (PPE).
| Course | Training | Responses | Response % |
|---|---|---|---|
| Dakar (February, 2015) | 30 | 10 | 33% |
| Dakar (October, 2015) | 28 | 17 | 61% |
| Ibadan (March, 2015) | 30 | 8 | 27% |
| Ibadan (September, 2015) | 33 | 18 | 55% |
| Accra (February, 2015) | 35 | 8 | 23% |
| Accra (November, 2015) | 35 | 9 | 26% |
Table 1: Course attendance between February 2015 and November 2015, in M-PACT courses.
A responding participant said: “I learnt about the high prevalence of TB in Nigeria, and how to be quick to rapidly assess patients. I also learnt about the new HIV national guidelines and how to chart a management plan in a patient who may be presenting with an infection. I also learnt that there is a wide differential list for a febrile ambulant patient, not just malaria. Lastly, but not least, I learnt about leadership.”
Another participant had this to say about the course and what he learned during the course:
“I learnt a teaching method based on clinical cases approach and I have been using it in teaching medical students and residents and also in my learning about diseases since my return to work.”
While a significant percentage of participants learned new things, it is important to note that 70.4% of all the respondents did not find it difficult to implement and apply the new concepts learned during the course.
However, new concepts learned that were difficult to implement at participants’ institutions/facilities included leadership role of doctors in the health care system, effective TB diagnosis, especially in children and people living with HIV and AIDS (PLHIVs). The widespread availability of “over-the-counter” antibiotics with abuse of drugs by patients altered the clinical picture of diseases, thereby sometimes confusing the attending physicians. Poor laboratory support made timely and accurate microbiological diagnosis impossible; infection control measures like hand washing was difficult to implement due to lack of running water and non-availability of antiseptic gel; and non-availability of personal protective equipment for routine ward procedures hindered their effective use.
In order of respondent frequency, non-communicable diseases, chronic kidney disease, cholera, multi-drug resistant TB, viral hemorrhagic fevers like Ebola and Lassa fever, dengue fever, pneumococcal meningitis, streptococcal meningitis, avian influenza, yellow fever, and viral hepatitides (hepatitis B and hepatitis C) were cited by respondents as emerging or reemerging epidemic diseases in the West African region.
To effectively implement M-PACT prevention strategies, the respondents identified several steps which include; (1) implementation of strict aseptic techniques in all healthcare units; (2) enforcing hand washing techniques and the use of protective clothing in all healthcare institutions and facilities; (3) emphasis on education, awareness and screening for TB, HIV and malaria with universal precautions among primary healthcare physicians; (4) proper and consistent use of PPE; (5) contact tracing of contacts of TB patients; and (6) stepping down of knowledge gained to other colleagues at participants’ work places.
One of the goals of the course was to train senior registrars to train and impact their locality and surrounding satellite primary healthcare facilities. Less than half of all participants (42.86%) had cascaded the training to their junior officers or medical students and impacted on the lower level of care in their localities as at the time of the survey.
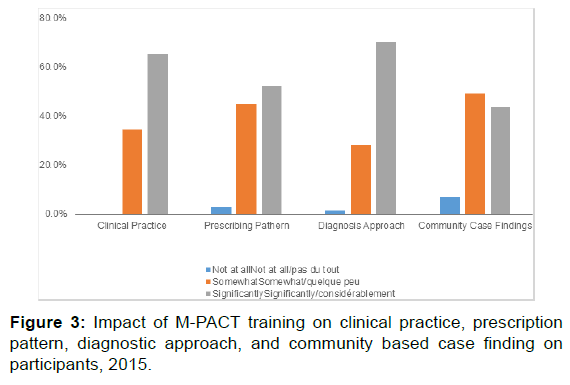
A number of participants had sessions with doctors from surrounding satellite institutions since their return from the course to update colleagues on better management and monitoring of TB and HIV or held (and are holding) discussions with healthcare workers in these outreach facilities. Since completing the course, many respondents found it easier to consult in the primary health care centers as they were able to prescribe more confidently, especially with respect to pediatric prescriptions. Another participant, who was in charge of an outstation of the hospital where he practiced, was able to implement testing for Malaria parasites using the Rapid Diagnostic Test (RDT) before prescribing drugs. However, not all were able to cascade the training to primary healthcare as one said, “I have only spread the link within my healthcare facility.” The survey revealed a 100 percent influence (significantly in 65.28%) on the clinical practice of participants; over 97% (significantly in 52.11%) on prescription patterns; over 98% on (significantly in 70.42%) diagnostic approaches; and over 91% (significantly in 43.66%) on case findings in the community (Figure 3).
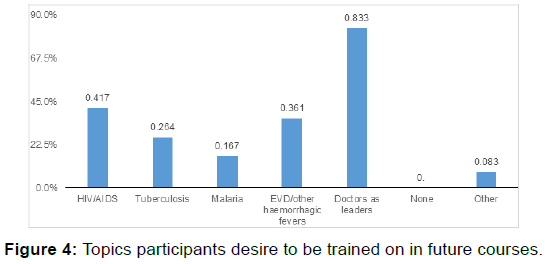
83.33% of all respondents identified training in leadership as a core need for future trainings and partnerships as shown in Figure 4.
Limitations
The short duration of the survey and the different intervals between various trainings and the evaluation for some cohorts may have impacted on number of participants who responded to the survey. Also, as most participants submitted their official, work e-mails, a change of job since M-PACT course with subsequent change of work/official email limited access to those who had moved on from their previous work places. Busy work schedules of most medical practitioners, poor access to internet, as well as low computer skills among physicians may also have limited the response rate. However, these may need further exploratory studies.
Discussion
The evaluation was well received and responses were very informative. From the responses, the M-PACT course made a difference in participants’ practices and helped develop new relationships. Although not all participants had used the skills and knowledge acquired very well, a large population of the trainees were building their career using knowledge and skills gained. A large percentage of the trainees suggested that leadership in health courses be made the focus of future partnerships.
The respondents were drawn from six different courses, but more participants in recent courses (September – November 2015) responded to the survey. This shows that, the sooner a survey is conducted, the more likely the participants will respond to it. The majority of respondents were drawn from the tertiary institutions which is also a reflection of their enrollment pattern as the emphasis of the course for the first two years was on the senior registrars drawn from the tertiary healthcare facilities.
That respondents were finding it difficult to implement some concepts learned in the course is an indication of the need for a system-wide change with involvement of healthcare institutions and facility managers in future trainings. Also, that a number of participants were yet to cascade the training to lower facilities indicates the need for post-training support to all participants towards translating the training from articles of faith to expressions of reality in and around their primary work places.
To ensure sustainability of the program in the West African subregion, the M-PACT course should be re-designed to provide continuous in-service personnel training for doctors and other healthcare workers. Secondly, the scope of M-PACT should be increased to provide training in other centers and for other categories of health workers. New partnerships that will address leadership in health, as well as infection control infrastructure should be established with the goal to build physician leaders in West Africa. Future courses should be decentralized to involve more centers and local capacity should be developed and/or strengthened to support the process in these other centers across West Africa. A decentralization of training to encompass all 16 nations in the sub-region with people accessing training close to where they live and work is critical and will significantly reduce the cost on the individual participants. It will also minimize need for bursaries for participants or payment made to participants.
Conclusion
We conclude that the format for the M-PACT course is popular and educationally instructive. The teaching portfolio would be useful for post-graduate medical training and career development not only in the countries of West Africa, but throughout sub-Saharan Africa.
Conflict of Interest
All authors disclose that there was no conflict of interest.
Acknowledgements
This article arose out of links forged through an Association of Physicians of Great Britain and Ireland “Links with Developing Nations” grant. SDT-R is grateful to the National Institute for Health Research (NIHR) Biomedical Facility at Imperial College London for infrastructure support. OOO acknowledges EFMC and IHVN for institutional support. The authors are grateful to Ecobank Foundation (Lomé, Togo) for funding support and to useful discussions with Professor Jane Dacre (President), Professor David Warrell (International Director) and Ms. Winnie Wade (Head of the Educational Unit) at the Royal College of Physicians of London. We also acknowledge the National training centers - University College Hospital, Ibadan, Oyo State, Nigeria; Korle Bu Teaching Hospital, Accra, Ghana; and Dakar Université Cheikh Anta DIOP de Dakar, Sénégal. Finally, we wish to acknowledge all the participants of M-PACT Courses in the centers that responded to the survey
REFERENCES
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2013 Jan 4;380:2095-2128.
- Lewden C, Drabo YJ, Zannou DM, Maiga MY, Minta DK, Sow PS, et al. Disease patterns and causes of death of hospitalized HIV-positive adults in West Africa: A multicountry survey in the antiretroviral treatment era. Journal of the International AIDS Society. 2014 Jun 4;17(1).
- Team WE. Ebola virus disease in West Africa—The first 9 months of the epidemic and forward projections. N Engl J Med. 2014 Oct 16;2014:1481-1495.
- Oleribe OO, Salako BL, Mourtalla KM, Akpalu A, Mc Connochie M, Foster M, et al. Ebola virus disease epidemic in West Africa: Lessons learned and issues arising from West African countries. Clinical medicine (London, England) 02/2015; 15(1):54-7. DOI:10.7861/clinmedicine.15-1-54
- Oleribe O, Oladipo O, Nwachukwu C, Abimbola A, Nwanyanwu O. The complicated and complex Ebola Viral Disease (EVD) in West Africa. American Association for Science and Technology (AASCIT). Volume 1, Issue 3 October 2014 online. ISSN: 2375-3803
- Oleribe OO, Margaret M, Crossey E, Robinson SDT. Nigerian response to the 2014 Ebola viral disease outbreak: Lessons and cautions. Pan African Medical Journal.2015; 22 Supp (1:13). 10 October 2015
- Ameh C, Adegoke A, Hofman J, Ismail FM, Ahmed FM, Van den Broek N. The impact of emergency obstetric care training in Somaliland, Somalia. International Journal of Gynecology & Obstetrics. 2012 Jun 30;117:283-287.
- Wyss K. An approach to classifying human resources constraints to attaining health-related Millennium Development Goals. Human Resources for Health. 2004 Jul 6;2:1.
- Qureshi AM. Case Study: Does training of private networks of family planning clinicians in urban Pakistan affect service utilization?. BMC International Health and Human Rights. 2010 Nov 9;10:1.
- Monkey Survey. https://www.surveymonkey.com/
- Microsoft Office. https://www.microsoft.com/en-ng/




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.