The Predictive Value of Quadruple Tests in the Second Trimester of Pregnancy in Identifying Pregnancy Complications
2 Zabol University of Medical Sciences, Zabol, Iran
3 Student of Medicine, Students Research Committee, Zabol University of Medical Sciences, Zabol, Iran, Email: tahghighatt1@gmail.com
Citation: Moghadam MN, et al. The Predictive Value of Quadruple Tests in the Second Trimester of Pregnancy in Identifying Pregnancy Complications. Ann Med Health Sci Res. 2018;8:139-142
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Four tests are performed on the 20th to 15th week of gestation . These tests include Triple Markers and Inhibin A Markers. Research has shown that abnormal levels of quadruple markers are useful in predicting side effects of pregnancy, and several studies have shown that there is a significant relationship between abnormal levels of four tests and preterm delivery, preeclampsia, pregnancy pressure, intrauterine growth restriction, and premature rupture of fetal curves. There are few previously published large studies that evaluated combination of quad screen markers,the aim of this study was to predict the predictive value of quadruple tests in the second trimester of pregnancy in the diagnosis of complications, especially the prediction of fetal death and abortion at birth. Method: This is a longitudinal study. All pregnant women in their second trimester who referred to Zabol city labaratory in 1995 and 1996 for Quad Marker testing were included. The exclusion criteria were: mothers over 35 years of age, mothers with a history of preterm labor, gestational hypertention and Down syndrome. Results: 240 pregnant women participated in this study. 29.2% of them were in the age group of 15 to 25 years old and 41.3% were in the age group of 31 to 35 years old. The results showed that only the surface area below the UE3 curve is statistically significant (AUC=0.144, p=0.007). The best UE3 value for detecting fetal death with a sensitivity of 100% and a 8% attribute equals 0.265 and the best AFP value for diagnosis of abortion with a sensitivity of 86% and 78% is 1,765. Discussion: In our study, although the underlying curve for Inhibin was higher than other markers, but the overlap between the confidence intervals for the surface under the curve of the three markers of Inhibin, Alfus, Protein and HCG indicated no significant difference in the level below the curve of the three markers. In a study by Duric et al., which was done by cohort method, 2384 pregnant women were evaluated in Croatia. The results of this study indicate that the increase in AFP was significantly associated with intrauterine growth retardation and spontaneous abortion, and the increase in HCG levels in the second trimester of pregnancy was associated with preterm delivery and intrauterine fetal death, as well as a decrease in the serum levels of 3 U.S. Mother in the second trimester of pregnancy is associated with preterm labor and restriction of uterine infertility.
Keywords
Quadruple tests; Pregnancy complications; AFF; Gonadotropin (hCG); Nonconjugate estradiol (UE3); Inhibin
Introduction
In broad terms, the term “high-risk pregnancy” refers to an increased risk of disability or mortality in, before, during, or after delivery of a mother, fetus, or new-born baby. Factors involved in high risk pregnancies include maternal health, abnormal midwifery and fetal illnesses. Ultimately, pregnancy can include maternal or fetal or infant mortality. The main causes of maternal mortality can include thromboembolic diseases, hypertension, bleeding, infection, and ectopic pregnancy. [1] The main causes of infant mortality (death from birth to age 1) include congenital anomalies, and the consequences of prematurity. Although there are differences according to the type of definition, all the deaths after the 25th week of pregnancy to 7 days after delivery are called perinatal deaths. The primary cause of perinatal illness and neonatal mortality is premature birth. Premature labour is a major problem in the medical community. [2] Congenital anomalies are the main cause of infectious diseases and infant mortality. Despite the many advances made in the care of newborns, preterm delivery is still a major cause of death in infants and causes important complications such as cerebral palsy and disability during school hours. [3] Annually millions of premature babies are born, accounting for approximately 75% of cases of perinatal mortality and morbidity. [4] Since the process of halting the preterm delivery or onset of labor has been less successful, today, researchers are more focused on predicting and preventing early delivery. The first step in preventing preterm labor is to predict it. In this regard, For prediction and screening of preterm delivery, various methods such as factors demographic, biological, serum markers and cervical markers and cervical dilatation have been introduced. [4] Triple trials have been also available since the early 1980s as Down Syndrome Screening Tests and Neural Tube Defects during pregnancy. AFF, gonadotropin (hCG), and non-conjugate estradiol (UE3) have three components of screening in the second trimester of pregnancy. [1] Since 2008, quadruple tests have become more subjective tests of trials. [5] Four tests are performed on the 20th to 15th week of gestation. [6] These tests include Triple Markers and Inhibin A Markers. Research has shown that abnormal levels of quadruple markers are useful in predicting side effects of pregnancy, and several studies have shown that there is a significant relationship between abnormal levels of four tests and preterm delivery, preeclampsia, pregnancy pressure, intrauterine growth restriction, and premature rupture of fetal curves. [7] There are few previously published large studies that evaluated combination of quad screen markers,the aim of this study was to predict the predictive value of quadruple tests in the second trimester of pregnancy in the diagnosis of complications, especially the prediction of fetal death and abortion at birth.
Research Methodology
This is a longitudinal study. All pregnant women in their second trimester who referred to Zabol city labaratory in 1995 and 1996 for Quad Marker testing were included. The exclusion criteria were: mothers over 35 years of age, mothers with a history of preterm labor, gestational hypertention and Down syndrome. Data on maternal delivery and maternal delivery, case study and outcome assessment were compiled in the checklist. Multivariate models with the highest fitness as predictive models of pregnancy outcomes were introduced. All statistical analyses were performed using Stata V.11 software.
Findings
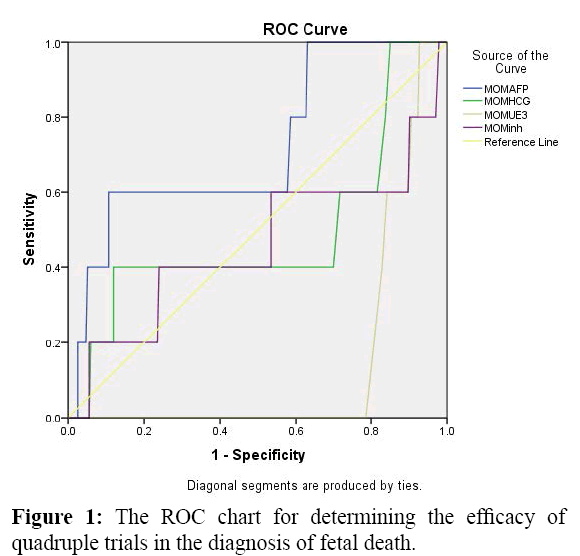
240 pregnant women participated in this study. 29.2% of them were in the age group of 15 to 25 years old and 41.3% were in the age group of 31 to 35 years old. Figure 1 compares the ROCs of the four diagnostic tests AFP, HCG, UE3 and Inhibin in the diagnosis of fetal death. As shown in Table 1, only the surface area below the UE3 curve is statistically significant (AUC=0.144, p=0.007).
| Quad tests | Area under the curve | P-value | 95% confidence interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| MOMAFP | 0.721 | 0.090 | 0.483 | 0.960 |
| MOMHCG | 0.488 | 0.930 | 0.180 | 0.796 |
| MOMUE3 | 0.144 | 0.007 | 0.085 | 0.204 |
| MOMinh | 0.460 | 0.759 | 0.144 | 0.776 |
Table 1: Level below the ROC curve to determine the efficacy of quadruple trials in detecting fetal death.
Table 2 shows that the best UE3 value for detecting fetal death with a sensitivity of 100% and a 8% attribute equals 0.265.
| Name of the Test | Optimum Point | Sensitivity | Speciality |
|---|---|---|---|
| AFP | 2.18 | 60% | 89% |
| HCG | 1.15 | 40% | 88% |
| UE3 | 0.265 | 100% | 8% |
| INH | 1.28 | 40% | 76% |
Table 2: Optical values for furrency tests for diagnosis of IUFD.
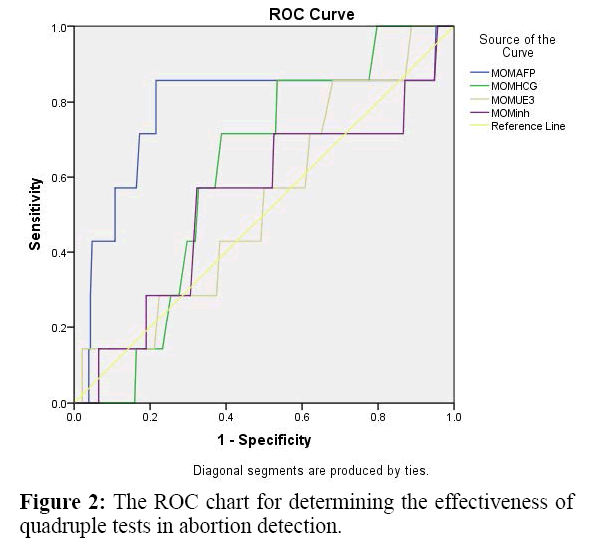
Figure 2 compares the ROCs of the four diagnostic tests AFP, HCG, UE3 and Inhibin in the diagnosis of abortion. As shown in Table 3, only the AFP curve below the other curves was higher and statistically significant (AUC=0.776, p=0.013).
| Quad Tests | Under Curve Area | P-value | 95% confidence interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| MOMAFP | 0.776 | 0.013 | 0.549 | 1.000 |
| MOMHCG | 0.612 | 0.311 | 0.460 | 0.765 |
| MOMUE3 | 0.532 | 0.771 | 0.330 | 0.735 |
| MOMinh | 0.539 | 0.727 | 0.304 | 0.774 |
Table 3: Level below the ROC curve to determine the efficacy of quadruple tests in abortion detection.
Table 4 shows that the best AFP value for diagnosis of abortion with a sensitivity of 86% and 78% is 1,765.
| Test Name | Optimum Point | Sensitivity | Speciality |
|---|---|---|---|
| AFP | 1.765 | 86% | 78% |
| HCG | 0.765 | 71% | 61% |
| UE3 | 0.485 | 57% | 50% |
| INH | 1.20 | 57% | 68% |
Table 4: Optimum values for each test in abortion detection.
Discussion
In this study, UE3=0.265, AFP=1.765, had the highest sensitivity and specificity in the prediction of fetal death, respectively, in abortion. In the study of Zahra Sehat et al., 700 pregnant women were diagnosed in the second trimester of pregnancy. 53 mothers (7.6%) had preterm labor. Sensitivity and specificity of the four tests for early delivery were 20.8% and 32%, respectively, which did not have a significant relationship with preterm labor. UE3 showed a significant statistical relationship with less than 0.8/0 MoM with early delivery. In this study, it was noted that the clinical use of this test in predicting preterm labor requires more extensive studies. According to Dugoff et al., If only an abnormal marker, there is a small, but significant relationship between the occurrence of pregnancy problems and abnormal marker levels. Also, if two or more of the markers are abnormal, the risk is likely to increase. One of the prevalence problems in this study was preterm delivery. Among the markers studied in this study, the highest correlation was observed with an increase in inhibitin A level (p=0.04). However, in our study, although the underlying curve for Inhibin was higher than other markers, but the overlap between the confidence intervals for the surface under the curve of the three markers of Inhibin, Alfus, Protein and HCG indicated no significant difference in the level below the curve of the three markers. In a study by Duric et al., which was done by cohort method, 2384 pregnant women were evaluated in Croatia. The results of this study indicate that the increase in AFP was significantly associated with intrauterine growth retardation and spontaneous abortion, and the increase in HCG levels in the second trimester of pregnancy was associated with preterm delivery and intrauterine fetal death, as well as a decrease in the serum levels of 3 U.S. Mother in the second trimester of pregnancy is associated with preterm labor and restriction of uterine infertility. [8,9] In the study of Walton et al., High levels of HCG in the mother’s serum were associated with an increase in the incidence of placental anomalies, stillbirth, gestational hypertension and early delivery. However, between levels of HCG with gestational diabetes, preeclampsia, and limited intrauterine growth there was no artifact. By considering racial categories and ethnicities in different groups, the predictive value of pregnancy problems has been superior to the predictive value of HCG alone. Finally, it was concluded that the measurement of maternal serum HCG has a small predictive effect on pregnancy outcomes. [3] In a study by Yaron et al., The findings indicate that AFP elevation is greater than 2.5 MOM=as the point Cut off was significantly associated with an increase in blood pressure induced by pregnancy, intrauterine fetal death, intrauterine growth restriction, abortion, preterm labor, oligohydramnios and early placental pairing. Increasing the serum HCG level was greater than 5/2 MOM=Significantly associated with elevated blood pressure, abortion, preterm labor, and intrauterine death, and finally, a decrease in serum estradiol level Conjugate with a level less than 0.5 MOM=associated with increased intrauterine fetal death, intrauterine growth restriction, embryo-induced hypertension, and concluded that the Multi-Marker screening test could not only be used for screening Down syndrome But also used to determine high-risk pregnancies. [10]
Conclusion
Among the four trials conducted during pregnancy, the UE3 test is the best predictor of fetal death. Of course, the predictive power of these tests was not excellent, but it can be said that they are good predictors of the outcomes of the pregnancy mentioned. Limitations of the study include a small sample size and possible selection bias.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Yazdani S, Rouholahnejad R, Asnafi N, Sharbatdaran M, Zakershob M, Bouzari Z. Correlation of pregnancy outcome with quadruple screening test at second trimester. Medical Journal of The Islamic Republic of Iran (MJIRI). 2015;29:1068-1075.
- Raeesian F, Lamiyan M, Hajizadeh E, Bakouie S, Soltanmoradi S, Moghaddam BL, et al. Serum zinc & iron in the first half of pregnancy and their relationship with preterm delivery: A prospective longitudinal study. 2015.
- Roghaei MA, Sabahi R, Ghasemi M. Studying the combination of cervical interleukins-6 and-8 with cervical dilatation in predicting preterm labor. 2009.
- Sehat Z, Goshetasbi A, Amin MT. Investigating association between second trimester maternal serum biomarkers and pre-term delivery. Iranian Journal of Reproductive Medicine. 2013;11:127.
- Shaw SS, Chen CP, Cheng PJ. From Down syndrome screening to noninvasive prenatal testing: 20 years' experience in Taiwan. Taiwanese Journal of Obstetrics and Gynecology. 2013;52:470-474.
- Walton DL, Norem CT, Schoen EJ, Ray GT, Colby CJ. Second-trimester serum chorionic gonadotropin concentrations and complications and outcome of pregnancy. New England Journal of Medicine. 1999;341:2033-2038.
- Lao MR, Calhoun BC, Bracero LA, Wang Y, Seybold DJ, Broce M, et al. The ability of the quadruple test to predict adverse perinatal outcomes in a high-risk obstetric population. Journal of medical screening. 2009;16:55-59.
- Dugoff L, HobbinsJC, Malone FD, Vidaver J, Sullivan L, CanickJA, et al. Quad screen as a predictor of adverse pregnancy outcome. Obstetrics &Gynecology. 2005;106:260-267.
- Duric K, Skrablin S, Lesin J, Kalafatic D, Kuvacic I, Suchanek E. Second trimester total human chorionic gonadotropin, alpha-fetoprotein and unconjugated estriol in predicting pregnancy complications other than fetal aneuploidy. European Journal of Obstetrics &Gynecology and Reproductive Biology. 2003;110:12-15.
- Yaron Y, Cherry M, Kramer RL, O’Brien JE, Hallak M, Johnson MP, et al. Second-trimester maternal serum marker screening: maternal serum α-fetoprotein, β-human chorionic gonadotropin, estriol, and their various combinations as predictors of pregnancy outcome. American journal of obstetrics and gynaecology. 1999;181:968-974.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.