Thrombocytosis in Under-Five Children with Lower Respiratory Tract Infection
Citation: Jasashree Choudhury. Thrombocytosis in Under-Five Children with Lower Respiratory Tract Infection. Ann Med Health Sci Res. 2017; 7: 47-51
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
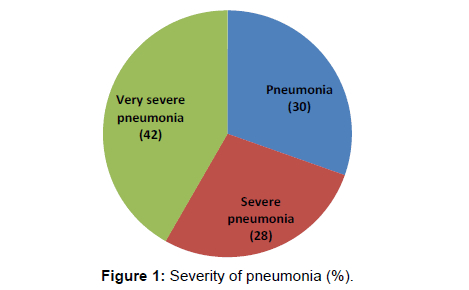
Background and aim: Thrombocytosis is a marker of inflammatory reaction with varied clinical conditions. The significance of thrombocytosis in relation to severity of the disease in under-five children with lower respiratory tract infection was evaluated. Method: It was a prospective observational study conducted during 12 months on 230 children within ages, 2 to 59 months, hospitalized for lower respiratory tract infection. Admitted patients were classified as children with and without thrombocytosis. Based on clinical severity patients were grouped; complications from thrombocytosis were analyzed and compared with those without thrombocytosis. Results: Of 230 children, 70 (30.4%) patients were with pneumonia, 64 (27.82%) were with severe pneumonia and 96 (41.7%) were with very severe pneumonia. Severity of pneumonia was more in infancy and 53.04% of total patients with pneumonia had thrombocytosis. The association between total leucocytes count and severity of pneumonia was significant. Thrombocytosis was seen in 82% case of pneumonia with pleural effusion. There was significant association of thrombocytosis with prolonged hospital stay. The mortality was 2.2% which had no significant association with thrombocytosis. Conclusion: Thrombocytosis is a frequent finding among children with lower respiratory tract infection. Children with thrombocytosis have more severe pneumonia with longer duration of hospitalization than those with normal platelet count. Platelet count may be used as a marker of disease severity and complication in children with lower respiratory tract infection.
Keywords
Lower respiratory tract infection; Thrombocytosis; Pneumonia
Introduction
Primary or essential thrombocythemia is extremely rare in the pediatric age group; but, infections at any body part including meninges are the common causes of reactive thrombocythemia in children. Besides acute infections, chronic inflammation, chronic hemolytic states and anemia are the other causes of pediatric thrombocytosis with a report of reactive thrombocytosis of 6 to 15% among hospitalized children. [1,2]. There are various studies suggesting thrombocyte count as a marker of serious bacterial infection. A studied incidence of reactive thrombocytosis among febrile young infants and assessed the utility of platelet count as a potential predictor of serious bacterial infection (SBI) in febrile young infants. [3]. A study revealed that upper respiratory tract infection as the most common cause followed by pneumonia as the infectious etiology of reactive thrombocytosis. [4]. Another study observed in their study that respiratory infection 28.3% was the predominant infectious cause of reactive thrombocytosis. [5]. An incidence and the clinical significance of thrombocytosis in children with lower respiratory tract infection caused by viral pathogens reactive. [6]. Thrombocytosis is a common finding in the acute care population of children hospitalized with viral lower respiratory tract infection. However a studied thrombocytosis after severe bacterial infections, particularly pneumonia with empyema in children. [7]. Similarly, evaluated platelet count in hospitalized patients with community acquired pneumonia and compared with abnormal leukocyte count and found that platelet count may be more informative in predicting poor outcome than abnormal leukocyte count. [8].
With the wide spread availability of automated analyzer in the field of hematology, we often get platelet count as component of routine hematology work up of every patient. As total platelet count has become a part of complete blood count. Higher frequency of thrombocytosis is being encountered in daily practice. The pathophysiology of reactive thrombocytosis involves evaluation of the level of thrombopoietin (TPO) and IL-6 along with other markers like IL-3, IL-11 and catecholamine’s which are produced in various inflammatory, infectious and neoplastic conditions. In situations of stress platelet play a major role in anti-microbial host defense, the induction of inflammation and tissue repair, activation of platelet enhance their interaction with complement proteins, humoral immune components as well as leucocytes and endothelial cells. Platelets bind, aggregate and internalize micro-organisms which hasten the clearance of pathogenic organism from the blood stream. They also take part in antibody dependent cell cytotoxicity to kill pathogen. Severe community acquired pneumonia is associated with significant increment in plasma level of inflammatory cytokines like TNF-alfa, IL-1B, IL6, IL8. The level of TNF-alfa, IL1B, IL6 were also elevated in the bronco alveolar lavage fluid of patients with community acquired pneumonia. [9]. Normal platelet count range between 1.5 Lakh to 4.5 Lakh /cmm and Platelet count of more than 5 Lakh /cmm common in infancy and childhood accounting in 3 to 13% of children. [10]. The estimated incidence of reactive thrombocytosis is 6-15% among hospitalized children. Infections of respiratory tract account for 60-80% of reactive thrombocytosis followed by infection of gastrointestinal tract and urinary tracts. Thrombocytosis is a quite common finding in infection of lower respiratory tract and children with thrombocytosis have a more severe presentation at admission and have a protracted clinical course resulting in longer duration of hospitalization than those with normal platelet count. [2].
Subjects and Methods
This study was a prospective observational study done in the department of pediatrics over a period of 1 year. All patients between 2 months to 59 months of age admitted with a clinical diagnosis of lower respiratory tract infection were studied. Patients were classified as per WHO criteria in ARI control programme guidelines. [11]. Those children with LRTI associated connective tissue disorders, congenital heart diseases, anemia (Hb<10gm)% were excluded from the study. After taking the consent from the parents demographic, clinical data and laboratory investigation results were collected for each participant. Complete blood count was performed with automated sysmex 6 part analyzer (N Series) and differential was checked by an experienced hematologist for any specific abnormality. The chest radiographs were reviewed by the radiologist. As per ARI control programme tachypnea was defined as respiratory rate more than 50/min in children two month to 12 months of age and more than 40 per minutes in children more than 12 month to 59 month of age. Respiratory distress was defined by the presence of either tachypnoea and or retraction of chest or oxygen saturation of <94% in room air. Clinical severity of the disease was classified as mild, moderate and severe distress. The outcome was measured as survival and death. The duration of hospitalization, admission to intensive care unit were noted. Thrombocytosis was considered when peripheral blood platelet count was more than 5 Lakh / cmm. Thrombocytosis is further divided into mild 5-7 Lakh/ mm3, moderate 7-9 Lakh/mm3 and severe 9-10 Lakh/mm3. All the patients were classified into two groups on the basis of thrombocyte count i.e., patients with or without thrombocytosis. All the variables were compared and statistical analysis was performed using the statistical package for the social science version 15 (SPSSINC, Chicago, USA). Results of analysis were provided as numbers, percentage or as mean ± standard deviation whenever applicable. Comparisons of the frequency of variables between patients with thrombocytosis and without thrombocytosis were made using chi-square test and students T-test. P-value of ≤ 0.05 was considered statistically significant [Figures 1 and 2]. [12].
Results
A total of 230 children were admitted with lower respiratory tract infection. 170, (73.9%) of cases were in the age group of two months to 12 months and rest 60 (26.1%) were between 13 months and 59 months. A total of 96 (45.7%) children were admitted with very severe pneumonia, 64 (27.82%) were severe pneumonia and 70 (30.4%) cases were with pneumonia. [Table 1].
| LRTI | Patients |
|---|---|
| Pneumonia | 70 |
| Severe pneumonia | 64 |
| Very severe pneumonia | 96 |
| Total | 230 |
Note: LRTI, Lower respiratory tract infection.
Table 1: Severity of pneumonia.
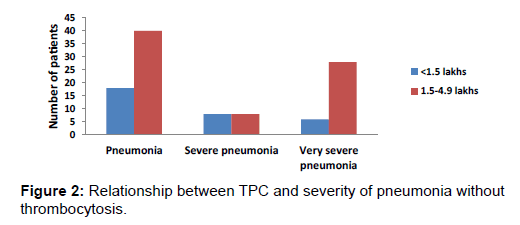
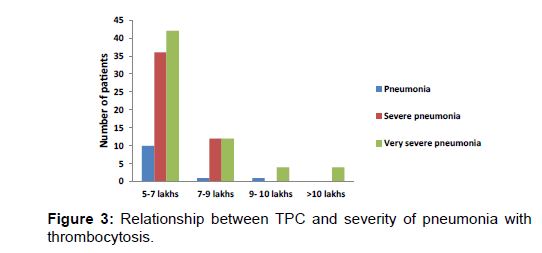
Out of 170 infants majority of cases (80) were admitted with very severe pneumonia followed by (52) with severe pneumonia and (38) were with pneumonia but in children in the age group of 13 to 59 months majority were admitted with pneumonia (32), (16) with very severe pneumonia and (12) with very severe pneumonia. This clearly depicts the severity of pneumonia more marked in the infants than in older children. Children from lower socio economic strata suffered from more severe pneumonia. Total 138 (60%) cases were undernourished whereas 92 (40%) children were having normal nutritional status. Severity of pneumonia increased significantly (P value <0.001) in children with malnutrition as compared to children with normal nutritional status. 85.6% of children with very severe pneumonia were undernourished and only 14.4% having normal nutritional status [Figure 1]. Thrombocytosis was found in 122 (53%) of all children admitted with pneumonia. 108 children had normal platelet count. Out of these 122 patients 76 (62.29%) were in the age group of 2 months to 12 months. This suggests thrombocytosis is more common in infants with lower respiratory tract infection. There was significant association between platelet count and severity of pneumonia. Among 5 children with severe of thrombocytosis (9-10 Lakh/ cmm) four had very severe pneumonia and one had pneumonia. All the four children with extreme thrombocytosis (> 10 Lakh/ cmm) had very severe pneumonia. This indicates association of severity of pneumonia with degree of thrombocytosis. [Table 2, Figures 3 and 4].
| Thrombocytosis | TPC in lakhs |
Pneumonia | Severe pneumonia | Very severe pneumonia |
Total patients |
*p-value |
|---|---|---|---|---|---|---|
| Without thrombocytosis | <1.5 | 18 | 8 | 6 | 32 | <0.001 |
| 1.5-4.9 | 40 | 8 | 28 | 76 | ||
| With thrombocytosis | 5-7 | 10 | 36 | 42 | 88 | |
| 7-9 | 1 | 12 | 12 | 25 | ||
| 9- 10 | 1 | 0 | 4 | 5 | ||
| >10 | 0 | 0 | 4 | 4 |
Note:*, Test of one- tailed significance.
Table 2: Relationship between platelet count and severity of pneumonia.
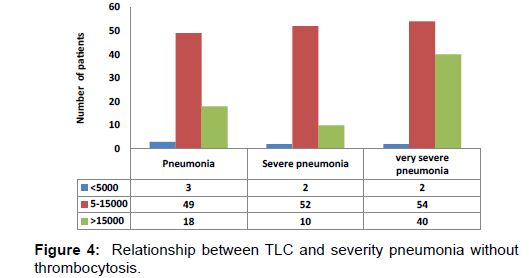
Significant association was seen between total leukocyte count and severity of pneumonia (P value -0.0086). The association between total leukocytes count and severity of pneumonia was significant. Out of 96 cases of very severe pneumonia 54(56.2%) had total leukocyte count between 5000-15000/cm2, 40 (41.6%) cases had total count of >15,000/cmm and 7 (2.08%) had total leukocyte count < 5000/mm3 [Table 3].
| TLC | Pneumonia | Severe pneumonia | Very severe pneumonia | Total patients |
*p-value |
|---|---|---|---|---|---|
| <5000 | 3 | 2 | 2 | 7 | 0.0086 |
| 5-15000 | 49 | 52 | 54 | 155 | |
| >15000 | 18 | 10 | 40 | 68 | |
| Total | 70 | 64 | 96 | 230 |
Note:*, Test of one- tailed significance.
Table 3: Relation between TLC and severity of pneumonia.
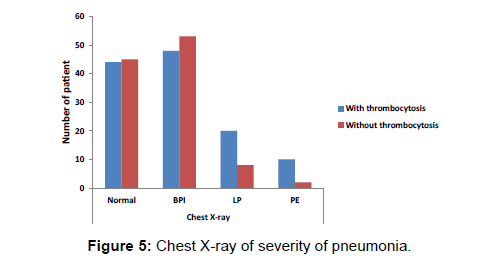
Out of 4 cases of severe thrombocytosis (9.01 – 10.00 Lakh/cmm) two case were of extreme thrombocytosis (>10 lakh/cmm) had TLC more than 15,000/cmm. With increasing in platelet count total leukocyte count was also increased. Significant association of thromobcytosis and leukocytosis with increasing severity of pneumonia was noted. Children with lobar pneumonia and synpneumonic effusion had very severe pneumonia. Significant association was marked between thrombocytosis and chest x-ray (P value -0.0099) [Table 4 and Figure 5].
| TPC | Chest X-ray | *p-value | |||
|---|---|---|---|---|---|
| normal | BPI | LP | PE | ||
| Without thrombocytosis | 45 | 53 | 8 | 2 | 0.0099 |
| With thrombocytosis | 44 | 48 | 20 | 10 | |
Note: *, Test of one- tailed significance; BPI, Bilateral pulmonary in filtralis; LP, Lobar pneumonia; PE, Pleural effusion.
Table 4: Chest x-ray of severity of pneumonia.
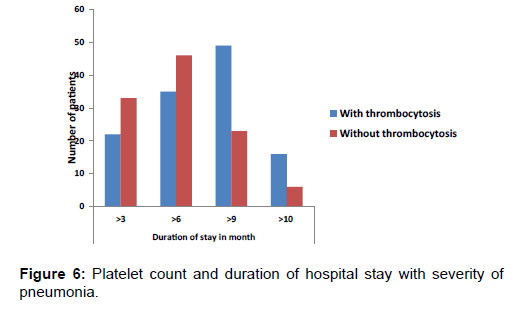
BPI-bronco pulmonary infiltrates, LP-lobar pneumonia, PEP leural effusion Out of 12 children with pleural effusion 10 (83.3%) cases had thrombocytosis. Out of 28 children with lobar pneumonia 20 (70.14%) cases had thrombocytosis. Most of the children with broncho pulmonary infiltrates in chest x-ray had platelet count with normal range. There was significant association of thrombocytosis with duration of hospitalization (P value-0.0008). Those children with thrombocytosis had longer duration of hospitalization which implies the more sever pneumonia in them. [Table 5]. Association of thrombocytosis with mortality was not statistically significant. Those all children who succumbed had moderate thrombocytosis.
| TPC | Duration of stay in day | Total patients |
p-value |
|||
|---|---|---|---|---|---|---|
| >3 | >6 | >9 | >10 | |||
| Without thrombocytosis | 33 | 46 | 23 | 6 | 108 | 0.0008 |
| With thrombocytosis | 22 | 35 | 49 | 16 | 122 | |
Note: *, Test of one- tailed significance.
Table 5: Relation between platelet count and duration of hospital stay.
Discussion
Platelets play a major role in anti-microbial host defense, the induction of inflammation and tissue repair. The mechanism by which infection invokes thrombocytosis has not yet been fully understood. During respiratory tract infection, there is increasing levels of inflammatory cytokines which heightens production of thrombocyte. Accurate assessment of the severity of pneumonia is the key to manage patients with community acquired pneumonia and acute respiratory infection [Figure 1]. Lower respiratory tract infections are the leading cause of under-five mortality. Case fatality rates tend to be high in young infants and young children so as the severity of disease. In present study, out of 230 subjects, 170 (73.9%) were in age group of less than 12 months. This is comparable to study done by where 71% of cases were under the age group of 12 months. Severity of illness was more in infancy which is supported by another study. [13,14]. As the severity of pneumonia increases, platelet count also increases. In present study, 13.9% had low platelet count, 33.0% had normal platelet count and 53% had thrombocytosis. Among children with thrombocytosis, 72.13% had mild thrombocytosis, 20.4% had moderate thrombocytosis, 4.09% had severe thrombocytosis and 3.2% had extreme thrombocytosis. This is comparable to studies done where mild thrombocytosis was seen in 72-86%, moderate thrombocytosis in 6-8%, severe thrombocytosis in 3%, and extreme thrombocytosis in 0.5%. [15,16]. Study done by. [15,16]. 48% of total admission with LRTI had platelet count >5.00 Lakhs/ mm3 and children with thrombocytosis had more serious illness (P-value<0.001). Study by noted severe symptoms in patients with thrombocytosis than in patients with normal platelet count (P-value 0.004). [17]. Out of total 230 cases, 5.38% of the cases had TLC<5000/mm3, 67.39% of the cases had TLC between 5000- 15000/mm3 and 29.56% of the cases had TLC>15000/mm3. This is comparable to a study where 3% of the cases had TLC <5000/ mm3, 73.2% had TLC between 5000 - 15000/ mm3, and 22.2% had TLC > 5000/mm3. [18]. All 4 cases of severe thrombocytosis and 2 cases of extreme thrombocytosis, had total Leukocyte count>15000/mm3. This suggests that, with increase in total leukocyte count, platelet count also increases (P-value<0.001). A study community acquired pneumonia showed that platelet count was strongly associated (P-value<0.009) with 30 day mortality, whereas no association was observed for leukocyte count (P-value 0.5114) and they concluded that an abnormal platelet count is a better predictor of outcome than an abnormal leukocyte count. Significant association was seen between thrombocytosis and pleural effusion (P-value 0.0099). [19]. Out of twelve children with pleural effusion, 10 (83.3%) cases had thrombocytosis which is comparable to many studies [Figure 6]. [7,16].
Significant association of thrombocytosis with duration of hospital stay was noted (P-value 0.0008). Children admitted with LRTI having thrombocytosis had longer duration of hospital stay, which indirectly indicate more severity of pneumonia which is similar to study by. [20]. Platelet count increases as the severity of pneumonia increases. Importantly, thrombocytosis occurs almost exclusively in children with pleural effusion.
Similar finding was noted in study done by Vlacha et al. [16]. where the association of thrombocytosis with length of hospital stays was significant (P-value 0.03). Similar results with P-value of 0.004. Association of thrombocytosis with outcome of children having LRI was not statistically significant (P-value 0.523) in the present study. [21]. This may be explained by the small sample size and very low mortality rate in this study.
Conclusion
Thrombocytosis is a common finding in children with lower respiratory tract infection particularly in infants. Children with thrombocytosis have more severe disease and longer duration of hospitalization. Degree of thrombocytosis is directly correlated with severity of the illness. Thrombocytosis is seen exclusively in children with complications like pleural effusion. We can conclude that platelet count may be used as a useful marker associated with severity of lower respiratory tract infection and its complications so as to prioritize patients in a developing country like ours.
Conflict of Interest
All authors disclose that there was no conflict of interest.
Author Contribution
DR and JC examined patients, collected clinical data; DR, JC and AM interpreted the findings and instructed JC and SR to prepare the draft manuscript. Finally all authors including RNP edited and approved the manuscript.
REFERENCES
- Marwaha N. Thrombocytosis as a predictor of serious bacterial infection. Indian Pediatrics Volume 47-November, 2010.
- Dame C, Sutor AH. Primary and secondary thrombocytosis in childhood. Brit J Haematol. 2005, 129: 165-177.
- Fouzas 1, Mantagou L, Skylogianni E, Varvarigou A. Reactive thrombocytosis in febrile young infants with serious bacterial infection. Ndian: pediatr. 2010; 47: 937.
- Ozcan C, Şayl TR, Koşan-Çulha V. Reactive thrombocytosis in children. Turk J Pediatr.2013; 55:411-416.
- Subramaniam N, Mundkur S, Kini P, Bhaskaranand N, Aroor S. Clinico-hematological study of thrombocytosis in children. ISRN Hematol. 2014 29: 389257.
- Haidopoulou K, Goutaki M, Lemonaki M, Kavga M, Papa A. Reaction thrombocytosis in children with viral respiratory tract infections. Minerva Pediatr. 2011: 63:257-262.
- Wolach B, Morag H, Drucker M, Sadan N. Thrombocytosis after pneumonia with empyema and other bacterial infections in children. Pediatr Infect Dis J. 1990: 9: 718-721.
- Atef A. Hesham A, Helmy A. Heba thrombocytosis at time of hospitalization is a reliable indicator for severity of CAP patients in ICU. Egyptian Journal of Chest Diseases and Tuberculosis. 2012; 61: 145-149.
- Greene C, Lowe G, Taggart C, Gallagher P, McElvaney N, O’Neill S. Tumor necrosis factor – Alfa converting enzyme: Its role in community acquired pneumonia. J Infect Dis. 2002; 186: 1790-1796.
- Klinger HM, Jelkmann W. Role of blood platelets in infection and inflammation. J Interferon Cytokine Res. 2002; 22:913-922.
- Park K. Parks Textbook of Preventive and Social Medicine.22nd edn. Banasidas Bhanot, Jabalpur (India), 2013.
- Vikas D, Sachdev A, Yadav SP. Practical Pediatric Hematology (IAP) 2nd edn.2012; p. 90-97.
- Tiewsoh K, Lodha R, Pandey RM, Kalaivani M, Broor S, Kabra SK. Factors determining the outcome of children hospitalized with severe pneumonia. BMC Pediatrics. 2009; 9:15.
- Usha D, Sudha RA. Significance of thrombocytosis in lower respiratory infections medpulse international medical journal, Sept 2014;9:470-475.
- Yohannan MD, Higgy KE, Al-Mashhadani SA, Santhosh-Kumar CR. Thrombocytosis. Etiologic analysis of 663 patients. Clin Pediatr (Philia) 1994;33:340-343.
- Vlacha V, Feketea G. Thrombocytosis in pediatric patients is associated with severe lower respiratory tract inflammation. Arch Med Res. 2006; 37:755-759.
- Unsal E, Aksaray S, Koksal D, Sipit T. Potential role of interleukin 6 in reactive thrombocytosis and acute phase response in pulmonary tuberculoso. Postgrad Med J 2005; 81: 604-606.
- Purcell K, Fergie J. Lack of usefulness of an abnormal white blood count for predicting a concurrent serious bacterial infection in infants and young children hospitalized with respiratory syncytial virus lower respiratory tract infection. Pediatr Infect Dis J 2007;26:311.
- Mirsaeidi M, Peyrani P, Aliberti S, Filardo G, Bordon J, Blasi F, et al. Thrombocytopenia and thrombocytosis at the time of hospitalization predict mortality in patients with CAP. Chest 2010;137:416-20s
- Sreenivasa B et al. Pediatrics. International Journal of Contemporary Pediatrics. Int J Contemp Pediatr. 2015 May; 2:103-107.
- Prina E, Ferrer M, Ranzani OT, Polverino E, Cilloniz C, Moreno E, et al. Thrombocytosis is a marker of poor outcome in community acquired pneumonia. Chest 2013,143:767-75.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.