True Umbilical Cord Knot Leading to Fetal Demise
- *Corresponding Author:
- Prof. Joseph Ikechebelu
P.O. Box 244, Nnewi, Anambra State, Nigeria.
E-mail: ji.ikechebelu@unizik.edu.ng
Abstract
The incidence of true knot of the umbilical cord is not only very low but it is often undiagnosed antenatally when present despite the availability of prenatal ultrasonography. When the true knot remains tight, it may impede the circulation of the fetus and may result to fetal death in utero especially in labor. We report a very uncommon case of true knot of the umbilical cord that ultimately led to a fetal demise. A 39‑year‑old booked G7 P5+1 with four living children, who booked for antenatal care at a gestational age (GA) of 17 weeks. The fundal height was compatible with the GA throughout pregnancy. An ultrasound done at a GA of 36 weeks showed normal findings. She had onset of labor at a GA of 40 weeks and 5 days following cervical ripening with two courses of 50 μg misoprostol inserted at the posterior fornix 6 h apart. The fetal heart tones were monitored using Doppler sonicaid. They remained normal throughout labor that lasted 13 h. She subsequently had spontaneous vertex delivery with poor Apgar score. The baby died immediately after birth. The umbilical cord was more than double the normal length and a true knot of the umbilical cord was diagnosed after delivery of the baby. We have reported a case of true umbilical cord knot in Nnewi, South‑East Nigeria. Although this entity can be diagnosed antenatally, current experience is limited to incidental observation and consequent fetal demise.
Keywords
Fetal demise, True knot, Umbilical cord
Introduction
The occurrence of true knot of the umbilical cord is very rare.[1] It may be defined as entwining of a segment of umbilical cord, usually without obstructing fetal circulation and commonly result from fetal slippage through a loop of the cord.[1]
Although the reported incidence of true knots of the umbilical cords ranges from 0.3% to 2%,[2-5] certain factors have been noted to increase its predisposition. These include long umbilical cords,[2,3] polyhydramnios,[2] small size fetuses,[2,3] male fetuses, gestational diabetes mellitus, monoamniotic twins, process of undergoing genetic amniocentesis[4] and multiparity.[5]
Most obstetricians are often concerned and perplexed about the exact time of formation of true knot of the umbilical cord. In general, the belief is that true knot of the cord is formed between 9 and 12 weeks of gestation.[1] This early gestation is a period where the amniotic fluid volume is relatively large.[1] Paradoxically, there is reported evidence of knot formation of the umbilical cord when a woman is undergoing labor.[6]
In the majority of cases, true knots of the umbilical cord occur without any clinical significance. However, in some rare occasion, there exists an association between umbilical cord knots and intrauterine fetal death as was seen in this case.
Case Report
Mrs. AC, a 39-year-old booked G7P5+1 with four living children, presented at the Life Specialist Hospital Limited, Nnewi and booked for antenatal care on 23/03/2011 at a gestational age (GA) of 17 weeks. There was no previous history of knotting of the umbilical cord except that her umbilical cords in the previous deliveries were said to be reasonably long. The index pregnancy was desired and spontaneously conceived and was well supported by the husband - a 34 year old trader. Her booking parameters were said to be normal. The booking weight was 140 kg, height 1.69 m, blood pressure 120 mmHg. The booking hemoglobin level was 10.5 g/dl and urinalysis showed no abnormality.
Her hemoglobin genotype is AA and blood group is O rhesus D positive. The venereal disease research laboratory test was non-reactive. She tested negative to Human immune-deficiency virus I and II. The fasting blood sugar and 2 h post prandial were normal. She received two courses, each of intermittent preventive therapy for malaria and tetanus toxoid at a GA of 22 and 28 weeks respectively.
The index pregnancy was essentially uneventful and ultrasound done at 36 weeks GA revealed normal findings. Doppler ultrasound was not done as it was not routinely done in the hospital. She was not a known hypertensive or diabetic. Her previous four confinements were uneventful.
Examination revealed a young lady in painful distress, afebrile, not pale and anicteric. There was no pedal edema. The pulse rate was 78 bpm, full volume and regular. The blood pressure was 110/70 mmHg. The heart sounds I and II were heard and there were no murmurs. The respiratory rate was 22 cpm. The chest was clinically clear.
The abdomen was enlarged and moved with respiration. There was no area of tenderness. The symphysio-fundal height was 39 cm. The lie was longitudinal, presentation cephalic and 4/5 palpable per abdomen. The fetal heart tone was 144 bpm. Vaginal examination revealed a closed cervical os that was uneffaced and at station - 3. A diagnosis of postdatism with unfavorable cervix was made. No ultrasound was done prior to cervical ripening.
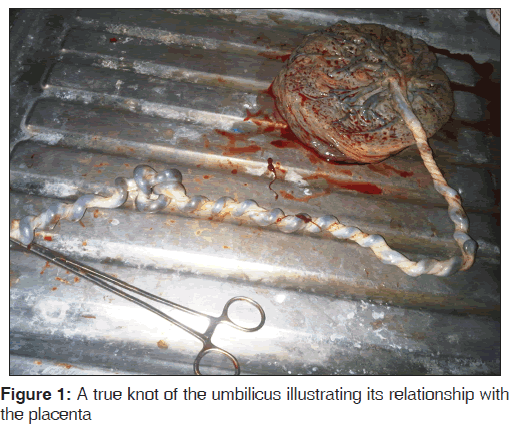
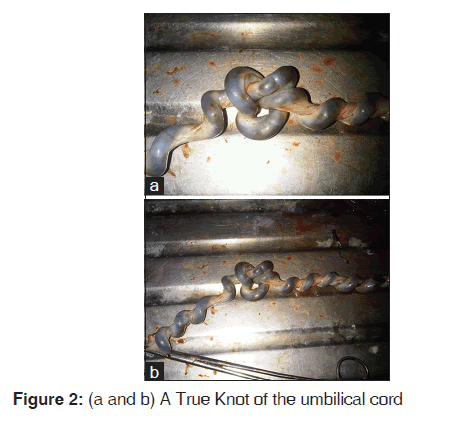
She subsequently had two courses of 50 μg of misoprostoland then transited into labor. The fetomaternal close monitoring was done and the mother and the baby showed no compromise. The fetal heart rate was monitored every 30 and 5 min in the first and second stages of labor respectively. At 12 h later, she had a spontaneous vertex delivery of a male baby that weighed 3.6 kg, Apgar score of 2 in 1 min. There was no retroplacental clot. The baby died immediately following delivery. The umbilical cord length was 126 cm. There was no gross fetal abnormality. The estimated blood loss was 200 ml. A true knot was found 7 cm distal to fetal insertion and the cord was found to insert centrally in the posterior placenta [Figure 1]. A diagnosis of true knot of the umbilical cord was made [See Figure 2].
Discussion
The diagnosis of true knot of the umbilical cord antenatally has not been commonly reported in the literature. This is the first reported case of true knot of the umbilical cord in Nnewi. In a previous study of umbilical cord knot involving 5575 deliveries which included 18 newborns with true knots, it was concluded that routine abdominal ultrasound for visualization of the abdominal insertion, cord-free and floating-free segments of the umbilical cord during evaluation of the amniotic fluid volume are insufficient for making the diagnosis of umbilical cord knot.[7] They arrived at such conclusion due to the following reasons. First, the second-trimester ultrasound scans performed in all the women were normal with no abnormality of the cord detectable. Second, 13 of the 18 women that finally had true knots also had color Doppler ultrasonography at the third-trimester, at which time the cord abnormality was secondarily missed prenatally. In one of these cases the diagnosis could have been made with color flow imaging, but multiple loops of cord was mistaken for abnormal pattern. Third, true knots were wrongly diagnosed prenatally in two cases, because they were not confirmed at delivery.[7]
A number of factors have been described to increase the predisposition to true umbilical cord. True knots may arise from movements of the fetus in utero. In the early pregnancy, this event is more likely to develop because relatively more amniotic fluid is present and greater fetal movement usually occurs. True knots are also associated with advanced maternal age, multiparity, male fetuses and long umbilical cords.[1,5,6] These factors are applicable to Mrs. AC, our patient. She was 39 years, grand multipara, delivered a male baby and had a very long umbilical cord. An average umbilical cord is 55 cm long, with a diameter of 1-2 cm and 11 helices. Despite this, the exact time the true knot occurred in the index case could not be ascertained.
Since the GA at which true knot actually occur is still unclear, true knots are difficult to diagnose prenatally. This is because, they have been reported to form in all three trimesters[6,7] and during scanning, the whole length of umbilical cord is not routinely seen. In addition, during the third trimester, parts of the cord may be obscured or concealed by the fetus; hence reliance on ultrasonography for diagnosis of true knot may be misleading. Some other researchers are of the opinion that true knots originate intrapartum and as such, there is no characteristic prenatal true knot appearance.[6,7]
Nevertheless, prenatal diagnosis of true knot of the umbilical cord has been demonstrated using ultrasound which will show “cloverleaf pattern” on gray scale images.[7,8] Although ultrasound was done for our patient, the diagnosis was missed. With prenatal ultrasound becoming more available in developing countries, expectation are that many affected fetuses will now be recognized prior to labor and this will allow the families and the obstetricians to be prepared for the birth of an affected child. Furthermore, following in utero diagnosis, prompt and close monitoring with cardiotocograph (CTG) can be done and urgent delivery will be carried out in the presence of abnormalities in the fetal heart rate tracing.[2,3]
A 4-fold increase in fetal loss have been reported to result from true knot, seemingly because the umbilical cord vessels can be compressed when the knot tightens.[1] This could explain the fetal demise observed in our present case.[1,6] False knots on the other hand, have no known clinical significance.[7-9]
Some conditions may enhance the prenatal detection of umbilical knots using ultrasonographic imaging. For instance, in monoamniotic twins where the true knot condition was purposely sought after.[8,9] However, despite the fact that the present case was that of singleton, our current experience is limited to incidental observation.
A cesarean delivery may be considered if a diagnosis of a true cord knot is made. Vaginal delivery is not usually encouraged although some obstetricians will view this differently. For instance, if the GA is near term, a trial of labor can be attempted, since the majority of knots seem to be protected against occlusion by the greater thickness of Wharton’s jelly and the large cord radius at this GA. If loose, a true knot will not lead to fetal compromise since fetal circulation is maintained.[1,7,8] However, at the time of fetal descent through the birth canal, the knot could be tightened. The tightening knot can occlude fetal circulation resulting in an intrauterine demise. Therefore, the Wharton’s jelly surrounding the fetal vessels has the potential of withstanding significant torsional and compressional forces. Occasionally, adequate Wharton’s jelly may not develop in all segments of the cord. When this occurs, the fetal vessels are no longer protected from torsional forces and they are prone to occlusion if twisted sufficiently leading to fetal demise in utero.[1,7] In this case report the newborn died after birth (1-min-Apgar: 2). This may suggest that the cause of death may have been triggered at the second stage of labor with little or no identification, considering that the fetal heart rate was closely monitored though intermittently. Besides, other possible reasons for the fetal demise could not be identified. The woman did not have retro placental blood clot and autopsy was not done.
In contrast to this recommendation, considerable levels of apprehension may exist between the parents and the obstetricians when attempts are made at attempting vaginal delivery. Retrospectively, in our case, delivery by caesarean section would have been justified. Thus, uncertainty lays the utility of antenatal testing in the follow-up of pregnancies with true knots.[10] Again, antenatal Doppler-sonography and subpartal continuous fetal heart rate tracing could also have been done for this woman.
Conclusion
As in our case, prenatal diagnosis of a true umbilical cord knot could be extremely difficult even with the use of ultrasonography for the reason that knots do not have characteristic prenatal ultrasonographic appearance. Furthermore, our current experience on true knot of the umbilical cord is limited to incidental observation. Therefore, there is a need for routine continuous monitoring of patients in labor using CTG.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Hershkovitz R, Silberstein T, Sheiner E, ShohamVardi I, Holcberg G, Katz M, et al. Risk factors associated with true knots of the umbilical cord. Eur J Obstet Gynecol Reprod Biol 2001;98:369.
- Spellacy WN, Gravem H, Fisch RO. The umbilical cord complications of true knots, nuchal coils, and cords around the body. Report from the collaborative study of cerebral palsy. Am J Obstet Gynecol 1966;94:113642.
- Airas U, Heinonen S. Clinical significance of true umbilical knots: A populationbased analysis. Am J Perinatol 2002;19:12732.
- Sherer DM, Dalloul M, Zigalo A, Bitton C, Dabiri L, Abulafia O. Power Doppler and 3dimensional sonographic diagnosis of multiple separate true knots of the umbilical cord. J Ultrasound Med 2005;24:13213.
- Sørnes T. Umbilical cord knots. Acta Obstet Gynecol Scand 2000;79:1579.
- Maher JT, Conti JA. A comparison of umbilical cord blood gas values between newborns with and without true knots. Obstet Gynecol 1996;88:8636.
- Sepulveda W, Shennan AH, Bower S, Nicolaidis P, Fisk NM. True knot of the umbilical cord: A difficult prenatal ultrasonographic diagnosis. Ultrasound Obstet Gynecol 1995;5:1068.
- Ramón y Cajal CL, Martínez RO. Fourdimensional ultrasonography of a true knot of the umbilical cord. Am J Obstet Gynecol 2006;195:8968.
- Deutsch AB, Miller E, Spellacy WN, Mabry R. Ultrasound to identify cord knotting in monoamniotic monochorionic twins. Twin Res Hum Genet 2007;10:2168.
- Stempel LE. Beyond the pretty pictures: Giving obstetricians just enough (umbilical) cord to hang themselves. Am J Obstet Gynecol 2006;195:88890.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.