Use of Oral Mucoperiosteal and Pterygo‑Masseteric Muscle Flaps as Interposition Material in Surgery of Temporomandibular Joint Ankylosis: A Comparative Study
- *Corresponding Author:
- Dr. Otasowie Daniel Osunde
Department of Dental Surgery, Maxillofacial Unit, University of Calabar Teaching Hospital, Calabar, Nigeria.
E-mail: dawn.foster@yale.edu
Abstract
Background: The most common complication of surgery for the release of temporomandibular joint (TMJ) ankylosis is relapse of the ankylosis. To prevent re‑ankylosis, a variety of interpositional materials have been used. Aim: The aim was to compare the surgical outcome of oral mucoperiosteal flap, not hitherto used as interpositional material, with pterygo‑masseteric muscles flap after surgical release of TMJ ankylosis. Subjects and Methods: This was a prospective randomized study of all consecutive patients treated for the release of complete TMJ bony ankylosis, from January 2003 to December 2012, at the Oral and Maxillofacial unit of our institution. The patients were randomized into two groups: The pterygo‑masseteric group comprises 22 patients while the oral mucoperiosteal group had 23 patients. Information on demographics, clinical characteristics, and postoperative complications over a 5 year follow‑up period were obtained, and analyzed using the statistical package for social sciences (Statistical Package for the Social Sciences version 13, Chicago, IL, USA). A P < 0.05 was considered significant. Results: The age of the patients ranged from 15 to 28 mean 20.3 (3.35) years while the duration of ankylosis ranged from 2 to 16 mean 5.1 (3.4) years. The baseline demographic (gender; P = 0.92; side; P = 0.58) and clinical characteristics in terms of etiology (P = 0.60) and age (P = 0.52) were comparable in both treatment groups. All the patients presented with complete bony TMJ ankylosis with a preoperative inter‑incisal distance of <0.5 cm. The intraoperative mouth opening achieved ranged from 4 cm to 5 cm, mean 4.6 (0.27) cm and this was not different for either group (P = 0.51). The patients were followed up postoperatively for a period ranging from 3 to 5 years, mean 3.4 (0.62) years. The mouth opening decreased, over the period of postoperative review, from the initial range of 4–5 cm to 2.9–3.6 cm, and this was not different in both groups (P = 0.18). Conclusion: This study suggests that oral mucoperiosteal flap could be an option in the choice of interpositional materials in surgery of TMJ ankylosis.
Keywords
Ankylosis, Interpositional materials, Temporomandibular joint
Introduction
Ankylosis of the temporomandibular joint (TMJ) involves fusion of the mandibular condyle to the glenoid fossa in the base of the skull, which causes distressing conditions such as impaired speech, difficulty in chewing, poor oral hygiene, facial disfigurement, compromise of the airway, and psychological stress.[1-4] Surgical treatment are aimed at improving esthetics, functional, and psychological well-being of the affected individuals as well as preventing re-ankylosis.[1-5] The most frequently reported complications after treatment of ankylosis are limited mouth opening, and re-ankylosis which occurs within 6 months postoperatively.[5] This re-ankylosis can be prevented by aggressive resectioning of the bony or fibrous tissues, especially in the medial aspect of the condyle, and by placement of interpositional materials.[6]
Many materials have been used for insertion at the ostectomy gap after resection of a bony segment: Alloplastic materials[7] (acrylic, Proplast–Teflon, Silastic), and autogenous tissues (temporalis muscle flaps, masseter-medial pterygoid muscles slings, dermis, costochondral grafts, and cartilage).[8,9] The several suggested materials only show that there is yet no ideal interpositional materials devoid of undesirable effects. Alloplasts as interpositional material may predispose the recipient site to infections or foreign body reactions.[5] In addition, there may be extrusion which may necessitate secondary procedures to retrieve the material. Long-term results of silicone sheet as an interpositional material revealed that 16.7% of the patients required second surgeries to remove the implants after an average interval of 5.6 years.[10] Other commonly used autogenous materials such as dermis, fascia lata and costochondra grafts, and cartilages are not vascularized in addition to the disadvantage of donor site morbidity. The temporalis muscle and fascia flap have been widely used for the reconstruction of the TMJ. In spite of its numerous advantages which include its autogenous nature, resilience, adequate blood supply, and proximity to the joint, it is not feasible in the intraoral TMJ arthroplasty.
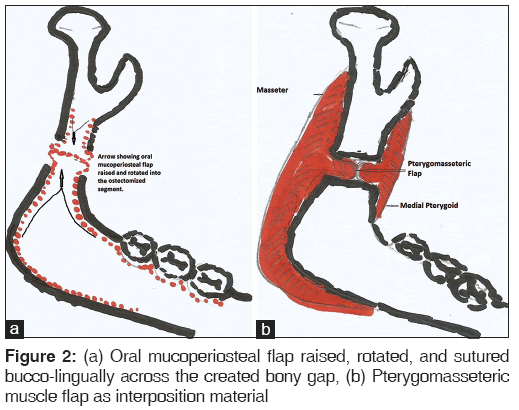
The pterygo-masseteric muscle flap as an interpositional material was first described by Eschmarc in the second half of the 19th century.[11] The advantages include anatomical proximity, vascularity and ease of suturing across the created joint. Although temporalis muscle and fascia flap is fast becoming the material of choice, pterygo-masseteric flap still plays a role as an interpositional material, especially when ramus or angle ostectomy is carried out. Oral mucoperiosteal flaps may also serve as an interpositional material because its qualities are comparable to that of pterygo-masseteric flap in terms of the vascularity, anatomical proximity, and the ease of suturing across the ostectomized segment.
To the authors’ knowledge, the use of oral mucoperiosteum as interpositional material has not been previously described as revealed by a literature search. The aim of this study was to compare treatment outcome using oral mucoperiosteal flap and pterygo-masseteric muscular flap as interpositional materials in surgery of TMJ ankylosis.
Subjects and Methods
This was a prospective randomized study of all consecutive patients treated for the release of complete TMJ bony ankylosis, from January 2003 to December 2012, at the Oral and Maxillofacial Unit, Department of Dental Surgery, of the University of Calabar Teaching Hospital. The criteria used for the diagnosis of complete bony TMJ ankylosis were: (1) Restricted mouth opening with maximal interdental distance of <0.5 cm; (2) absence of palpable movement at one or both condylar head, and (3) presence of bony consolidation in the region of the TMJ, on posterio-anterior, lateral oblique mandible, and TMJ radiographic views (Transcranial). Although computed tomography-Scan has become the gold standard in radiologic diagnosis of TMJ ankylosis, poverty among our patients precludes its routine use for diagnosis of TMJ ankylosis in our center. All selected patients underwent the interpositional gap arthroplasty with interpositional material varying between muscles and oral mucoperiosteum. The study protocol was approved by the Ethics Committee of our institution. A written consent was obtained from all the selected participants after adequate explanation of the study protocol.
Randomization
All consecutive patients who presented to the Oral and Maxillofacial unit of our institution with complete bony ankylosis (<0.5 cm) of the TMJ were consecutively randomized into two treatment groups as they present. In the first group, pterygo-masseteric muscles flap was placed as interpositional material (control group) and in the second group oral mucoperiosteal flap was interposed in the ostectomized segments (experimental group).
Surgical technique
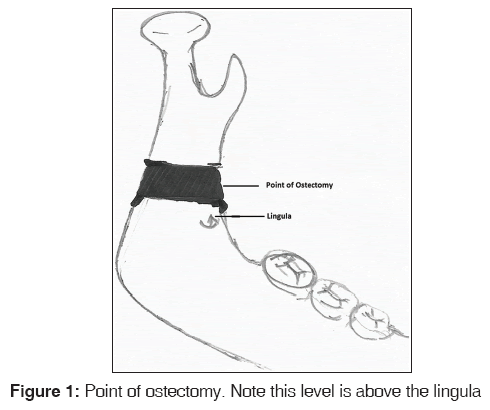
All procedures were carried out using intraoral approach by the same surgeon and assistant in the same operating theatre. To facilitate intubation, all patients required elective tracheostomy under local anesthesia because of lack of fiber optic laryngoscope in our institution. Under general anesthesia, the lateral surface of the angle-ramus region of the mandible was accessed through a gingival marginal incision starting from the disto-buccal angle of the 2nd molar continues posterio-laterally along the anterior border of the ramus and external oblique ridge and continues superiorly to the occlusal plane of the mandibular and maxillary teeth. A mucoperiosteal flap was then raised to expose the molar-angle-ramus region up to the sigmoid notch. With adequate soft tissue retraction and placement of protective flat metal instrument (periosteal elevator about 2.5 cm wide) beneath the mandible, osteotomies were carried out above the lingula in all the cases [Figure 1], using a mallet and an osteotome in combination with bone rongeur where necessary to create a gap of about 1.5–2 cm. In all the cases, the initial bone cut was carried out in steps rather than through and through and then completed with a bone rongeur. This was necessary in order to prevent injury to any adjoining neurovascular bundle. Mouth opening was achieved by osteotomy/ostectomy in combination with coronoidectomy when the initial mouth opening achieved was <3 cm. This inter-incisal distance was further improved using mouth crank, which also enhanced the surgical access. When adequate mouth opening has been achieved, the surgical site was thoroughly irrigated; interpositional materials were placed depending on the treatment group. In the experimental group, the mucoperiosteum related to the created gap was raised, rotated, and sutured medio-laterally across the gap as an interpositional material [Figure 2a]. Pterygo-masseteric muscle flap was sutured across the gaps as interpositional material in the control group [Figure 2b]. After adequate toileting and achievement of hemostasis, the reflected mucoperiosteal flaps in the control group, and the remainder in the experimental group were opposed using 3/0 black silk sutures. Using this protocol, an inter-incisal distance of 4–5 cm was achieved intraoperatively in all the cases. Both groups were placed on the same antibiotics and analgesics except for the choice of interpositional material as described. Parenteral ampiclox 500 mg 6 h, metronidazole 500 mg 8 h and pentazocine 30 mg 6 h were given for the first 48 h, and continued with oral clindamycin 150 mg 12 h and oral naproxen sodium 550 mg 12 h for 10 days. After completion of the above regimen, patients were advised to continue with Paracetamol 1000 mg 8 h when necessary.
Postoperative jaw exercises and follow-up
Jaw exercises began 48 h postoperatively and were vigorously carried out to the limit of patients’ tolerance. Our protocol involved use of stacks of wooden spatulas to open the mouth 6–8 times a day with each session lasting a minimum of 30 min. In between each active session patients were encouraged to continue the mouth opening exercises by chewing sugar-free gums. Patients were reviewed daily for the first 7–10 days and then discharged to continue follow-up on out-patient basis. Post discharge follow-ups continued biweekly for the 1st month and then monthly up to the 1st year. Thereafter patients were reviewed every 3 months for the first 2 years and then 6 monthly up to 5 years postsurgery. Patients who did not attain a minimum of 3 years postoperative follow-up were excluded from the study.
At each postoperative review section, the mouth opening was measured to determine the maximal interincisal distance. Using the criterion defined by Ansari et al.,[12] re-ankylosis was diagnosed when the mouth opening was <1.9 cm. Other evaluated parameters included occlusal anomaly which in this context, referred to malocclusion on both static, vertical, and on lateral excursion as well as deviation of the chin on opening or closing the mouth. The maximum inter-incisal distance and the lateral excursion were assessed clinically with ruler that was calibrated in millimeter. The measurements were carried out by the same examiner three times during each postoperative visit and the average taken to eliminate intra-observer error or discrepancies. Injury to the facial nerve, especially the buccal and the marginal mandibular branches were assessed by asking the patient to blow their cheek, purse the lip, and to smile. Inability to blow the cheek, purse the lip, or deviation of the lower lip indicated damage to these branches of the facial nerve. Loss or altered lower labial sensation indicated inferior alveolar nerve damage. In addition, serial plane radiographs were done at 1-month postsurgery; and then, at 6 monthly intervals up to 5 years postoperatively.
Statistical analysis
The data were analyzed using the statistical package for social sciences (Statistical Package for the Social Sciences version 13, Chicago, IL, USA). Categorical variables were presented as frequencies and percentages while continuous variables were presented as mean and standard deviations. Inferential statistics were done using Chi-square and independent t-tests as appropriate. A P < 0.05 was considered significant.
Results
A total of 48 patients with TMJ ankylosis was seen within the period of study. Three patients were excluded from the analysis because the duration of their postoperative follow-up was <3 years. Of the 45 patients who met the inclusion criteria, 23 had oral mucoperiosteal flap as interpositional material while the remaining 22 were done with pterygo-masseteric muscle flap. The age of the patients ranged from 15 to 28 mean 20.3 (3.35) years while the duration of ankylosis ranged from 2 to 16 mean 5.1 (3.4) years. The baseline demographic and clinical characteristics of both groups were comparable [Table 1]. Trauma (40/45 [88.9%]) and middle ear infections (5/45 [11.1%]) were the observed etiologic factor for the development of TMJ ankylosis in this study.
| Variables | Mucoperiosteum (n=23) | Muscles (n=22) | χ2 | P |
|---|---|---|---|---|
| Gender | ||||
| Female | 7 | 7 | 0.01 | 0.92 |
| Male | 16 | 15 | ||
| Aetiology | ||||
| Trauma | 21 | 19 | 0.27 | 0.60 |
| Infection | 2 | 3 | ||
| Side | ||||
| Left | 12 | 9 | 1.08 | 0.58 |
| Right | 7 | 10 | ||
| Bilateral | 4 | 3 | ||
| Contralateral | ||||
| coronoidectomy | ||||
| Yes | 5 | 4 | 0.09 | 0.77 |
| No | 18 | 18 | ||
| Mean (SD) | T | |||
| Age (years) | 20.6 (3.4) | 19.9 (3.3) | 0.7 | 0.5 |
| Follow-up (years) | 3.5 (0.6) | 3.2 (0.6) | 1.4 | 0.2 |
All data in frequency except where otherwise stated. SD: Standard deviation
Table 1: Demographic and clinical characteristics of study groups
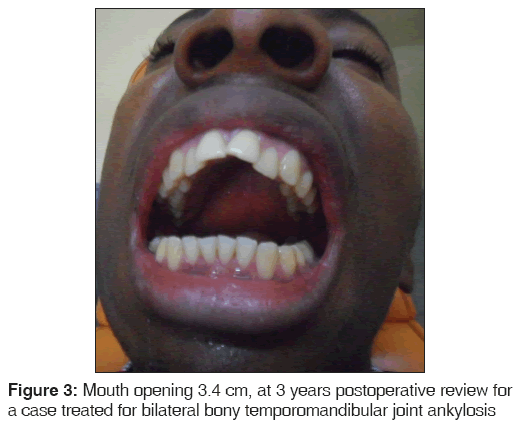
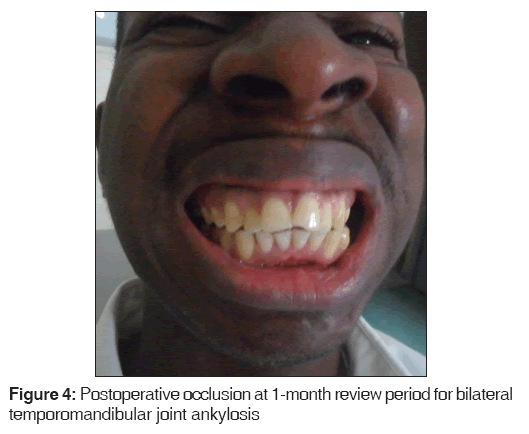
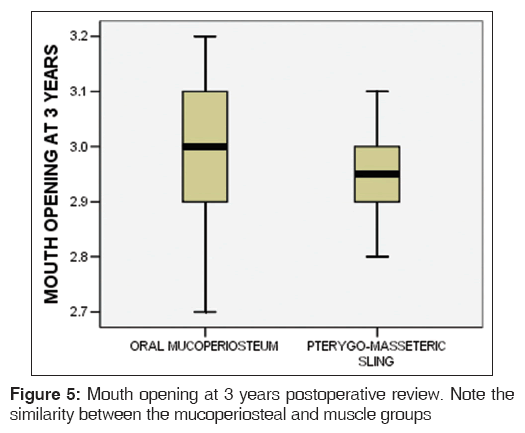
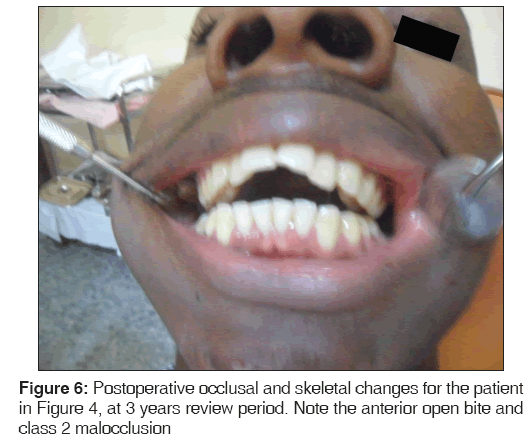
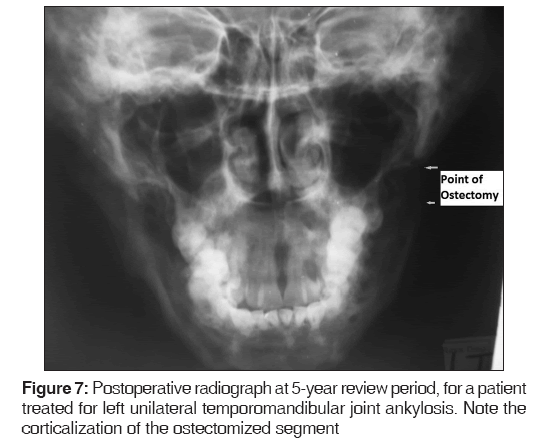
All the patients presented with complete bony TMJ ankylosis with a preoperative inter-incisal distance of <0.5 cm. The immediate or intraoperative mouth opening achieved ranged from 4 to 5 mean 4.6 (0.27) cm and this was not different for either group (t = 0.66, df = 43, P = 0.51). There were no intra-operative complications observed during the study. The patients were followed-up postoperatively for a period ranging from 3 to 5 years, mean 3.4 (0.62) years. There was a decrease in the intraoperative mouth opening, over the period of postoperative review, from the initial range of 4–5 cm to 2.9–3.6 cm [Figure 3]. This reduction in mouth opening was observed throughout the study period, and it occurred uniformly across both treatment groups. Presurgery lateral excursion was 0 cm for both groups. The occlusion, at 1 month postoperatively, was stable without the derangement in both groups [Figure 4]. At 3 years, the mean lateral excursions was not different for both treatment groups and these were estimated at 0.7 (0.15) cm bilaterally postsurgery in both unilateral and bilateral ankylosis. Furthermore, at 3 years postoperative review, the mouth opening were essentially the same in both the oral mucoperiosteum (3.0 cm) and the pterygo-masseteric muscle groups (2.9 cm) [Figure 5]. However, there were anterior open bite and Angle class 2 division 1 malocclusion in bilateral ankylosis [Figure 6], while unilateral cases presented with premature occlusion on the ipsilateral side and a cross bite on the contralateral side. At 5-year postoperative radiographic evaluation of a left unilateral case, the ostectomized segment was still intact, and the margins have been corticalized [Figure 7]. There was no injury to either the facial or the inferior alveolar nerves. Due to financial constraints nothing was done to correct the occlusal anomalies and facial deformity.
Discussion
The most common complication of surgery for the release of TMJ ankylosis is relapse of the ankylosis. To prevent re-ankylosis, a variety of interpositional materials have been used which include temporalis muscle and fascia, the dermis, auricular cartilage, fascia lata, fat, lyo-dura, silastic, silicone, and various metals.[13-17] While majority of the autogenous materials are associated with donor site morbidity, the alloplastic materials have been linked with infections at the recipient site, foreign body reactions and extrusions.[5] In the present study, we proposed the use of oral mucoperiosteal flap as an interpositional material and compared the results with pterygo-masseteric muscle flap which is one of the earliest documented material used in interpositional gap arthroplasty.
The results of the mouth opening achieved and occlusal derangement when the treatment techniques were compared at the end of the postoperative review period were similar. The reduction in mouth opening occurred uniformly across both study population over time. This reduction in mouth opening may be explained in terms of healing contractures as documented in several studies.[6,11,18] Apart from healing contractures reduction in mouth opening may also be due to fibrous or bony re-ankylosis.[5,6] The dimension of the initial passive mouth opening achieved at surgery without application of undue force, aggressive resection of the ankylotic mass as well as consistent postoperative mouth opening exercises have been reported as the main determinant factors for the prevention of re-ankylosis.[6,9,18] In this series, no case of re-ankylosis was recorded over the period of follow-up, both clinically and radiographically, probably due to the initial mouth opening achieved at surgery, estimated at 4–5 cm as well as the presence of interpositional material at the created bony gaps. Absence of re-ankylosis may also have been due to the high level of patients’ compliance with the postoperative jaw exercises which led to corticalization of the ostectomized segments.[19] The other reason may not be unconnected with the ages of the subjects, with the youngest being 15 years. Older patients may obviously tolerate the postoperative mouth opening exercises more than children due to differences in the level of pain threshold.
The malocclusion recorded in the two treatment groups and in unilateral, and bilateral ankylosis are consistent with previous reports.[5,20] As previously reported, this malocclusion including the reduced lateral mandibular excursion is due to healing contractures, reankylosis, retrusion of the mandible following ostectomy and it is synonymous with techniques that results in shortening of ramus of the mandible.[2,3,5] However the anterior open bite or ipsilateral premature contact with contralateral cross bite as it occurs in bilateral and unilateral TMJ ankylosis respectively, is less with techniques that restores the anatomical height of the ramus using either autogenous or alloplastic material.[5,12,18] Unfortunately, due to financial constraints on the part of these patients, the abnormalities including facial disfigurement were not corrected during the follow-up period. The subjects have decided to come to terms with their deformities.
Oral mucoperiosteal flaps like other previously reported flaps used in interpositional arthroplasty have the advantages of being vascularized, ease of suturing across the created false joint, and in addition its anatomical proximity to the surgical site. There may not be additional morbidity to the donor site since the interposed segment is part of the mucoperiosteal flap raised to expose the mandibular body-angle-ramus regions. Our choice of intraoral approach in the treatment of TMJ ankylosis in this study confers additional advantages compared to the conventional extraoral surgical approach. Ko et al.[21] previously reported on the release of TMJ ankylosis through intraoral approach and the results were excellent with no re-ankylosis. Intraoral endoscopic approach to the TMJ has also been described by Sembronio et al.[8] In this technique, the ankylotic bone excision was performed through the pre-auricular access and the resection was completed intraorally, with endoscopic assistance, using a piezoelectric osteotome. Our technique differed slightly in that the site of the ostectomy in the present study was lower without excision of the ankylotic mass.
The advantages of intraoral arthroplasty are absence of facial scar, reduced risk of injury to the facial and the auriculotemporal nerves, absence of sialocoele, reduced hemorrhage as well as the possibility of carrying out coronoidectomy or coronoidotomy through the same surgical access.[9,22] The reduced hemorrhage may partly be due to reflection of soft tissues away from the medial surface of the ramus above the lingula and thus protecting the maxillary artery from the surgical field.[21] Additional blood loss may arise from transection of subcutaneous and other vessels related to the extraoral lines of incision. The main draw-back of intraoral arthroplasty is the limited field of surgery and the high level of dexterity required by both the operator and assistant.[22]
Conclusion
This study has demonstrated the use of oral muccoperiosteal flap as an interpositional material. Because of the relatively small sample size of our study population, we suggest further studies with lager sample sizes and over a longer follow-up period to validate the findings of the present study.
References
- Posnick JC, Goldstein JA. Surgical management of temporomandibular joint ankylosis in the pediatric population. Plast Reconstr Surg 1993;91:791-8.
- López EN, Dogliotti PL. Treatment of temporomandibular joint ankylosis in children: Is it necessary to perform mandibular distraction simultaneously? J Craniofac Surg 2004;15:879-84.
- Chidzonga MM. Temporomandibular joint ankylosis: Review of thirty-two cases. Br J Oral Maxillofac Surg 1999;37:123-6.
- Qudah MA, Qudeimat MA, Al-Maaita J. Treatment of TMJ ankylosis in Jordanian children – A comparison of two surgical techniques. J Craniomaxillofac Surg 2005;33:30-6.
- Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg 1990;48:1145-51.
- Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg 2001;30:189-93.
- Bello SA, Aluko Olokun B, Olaitan AA, Ajike SO. Aetiology and presentation of ankylosis of the temporomandibular joint: Report of 23 cases from Abuja, Nigeria. Br J Oral Maxillofac Surg 2012;50:80-4.
- Sembronio S, Albiero AM, Polini F, Robiony M, Politi M. Intraoral endoscopically-assisted treatment of temporomandibular joint ankylosis: Preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:e7-10.
- Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg 2009;67:1966-78.
- Schliephake H, Schmelzeisen R, Maschek H, Haese M. Long-term results of the use of silicone sheets after diskectomy in the temporomandibular joint: Clinical, radiographic and histopathologic findings. Int J Oral Maxillofac Surg 1999;28:323-9.
- Huang IY, Lai ST, Shen YH, Worthington P. Interpositional arthroplasty using autogenous costal cartilage graft for temporomandibular joint ankylosis in adults. Int J Oral Maxillofac Surg 2007;36:909-15.
- Ansari SR, Iqbal S, Aslam S. Surgical correction of TMJ ankylosis – A study on the incidence and evaluation of success rates of various surgical procedures. Pak Oral Dent J 2003;23:105-12.
- Chossegros C, Guyot L, Cheynet F, Blanc JL, Gola R, Bourezak Z, et al. Comparison of different materials for interposition arthroplasty in treatment of temporomandibular joint ankylosis surgery: Long-term follow-up in 25 cases. Br J Oral Maxillofac Surg 1997;35:157-60.
- Chossegros C, Guyot L, Cheynet F, Blanc JL, Cannoni P. Full-thickness skin graft interposition after temporomandibular joint ankylosis surgery. A study of 31 cases. Int J Oral Maxillofac Surg 1999;28:330-4.
- Karaca C, Barutcu A, Menderes A. Inverted, T-shaped silicone implant for the treatment of temporomandibular joint ankylosis. J Craniofac Surg 1998;9:539-42.
- Matukas VJ, Lachner J. The use of autologous auricular cartilage for temporomandibular joint disc replacement: A preliminary report. J Oral Maxillofac Surg 1990;48:348-53.
- Paterson AW, Shepherd JP. Fascia lata interpositional arthroplasty in the treatment of temporomandibular joint ankylosis caused by psoriatic arthritis. Int J Oral Maxillofac Surg 1992;21:137-9.
- Sadakah AA, Elgazzar RF, Abdelhady AI. Intraoral distraction osteogenesis for the correction of facial deformities following temporomandibular joint ankylosis: A modified technique.
- Adekeye EO. Ankylosis of the mandible: Analysis of 76 cases. J Oral Maxillofac Surg 1983;41:442-9.
- Matsuura H, Miyamoto H, Ogi N, Kurita K, Goss AN. The effect of gap arthroplasty on temporomandibular joint ankylosis: An experimental study. Int J Oral Maxillofac Surg 2001;30:431-7.
- Ko EC, Chen MY, Hsu M, Huang E, Lai S. Intraoral approach for arthroplasty for correction of TMJ ankylosis. Int J Oral Maxillofac Surg 2009;38:1256-62.
- Khadka A, Hu J. Autogenous grafts for condylar reconstruction in treatment of TMJ ankylosis: Current concepts and considerations for the future. Int J Oral Maxillofac Surg 2012;41:94-102.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.