Usefulness of Prostate Specific Antigen Density in Prostate Cancer Detection among Men with PSA of 4-10 ng/ml
Citation: Agbo CA, et al. Usefulness of Prostate Specific Antigen Density in Prostate Cancer Detection among Men with PSA of 4-10 ng/ml. Ann Med Health Sci Res. 2020;10:1138-1141
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Prostate cancer (CaP) is a common malignancy in men and late presentation is still an issue. The discovery of PSA has revolutionized the diagnosis of CaP however has difficulties in discriminating malignant and benign prostatic status especially in patients with grey zone of 4.0-10.0ng/ml. Prostate specific antigen density is useful in this group of individuals. Aims and Objectives: To determine the usefulness of prostate specific antigen density (PSAD) in detection of prostate cancer in native African men with intermediate prostate specific antigen (4.0-10.0ng/ml). Design of the study: It was a cross-sectional, prospective study. Setting: This study took place at the Jos University Teaching Hospital, Urology Division, Department of Surgery, Jos, Nigeria. Materials and Methods: Men who presented at the urology clinic of Jos University Teaching Hospital with intermediate PSA of 4-10ng/ml that had either abnormal DRE findings or PSA density ≥0.15ng/ml² were recruited. Prostate volume was measured using ellipsoid formula through transabdominal ultrasound scan (a GE logic S expert 052128 model ultrasound). The PSA density was calculated by dividing PSA by prostate volume. They subsequently had digitally guided transrectal prostate biopsy. Results were recorded in a structured proforma. Statistical analysis was done using SPSS(R) version 20 (SPSS, IBM, Chicago, IL, USA). Appropriate test statistics were used with p-value < 0.05 considered as significant. Results: Seventy-two (72) men aged 47-99 years were enrolled in the study. The mean age at presentation was 65.4 ± 10.4 years. The cancer prevalence was 26.4%. The commonest age group with cancer was 60-69 years with a mean age of 68.4 years. At a cut-off of 0.15ng/ml2, the cancer detection rate, sensitivity and specificity of PSAD was 51.5%, 89.5% and 69.8% respectively (p <0.001). However, at cut-off of 0.12 ng/ml2, the PSAD had a sensitivity and specificity of 95.0% and 62.0% respectively with AUC 0.84 on ROC (p <0.001). Conclusion: PSAD showed statistical significance in cancer detection (p <0.001) with a detection rate, sensitivity and specificity of 51.5%, 89.5% and 69.8% respectively. It showed a higher sensitivity (95%) at a cut-off of 0.12. PSAD is thus useful in prostate cancer detection among men with PSA 4-10 ng/ml.
Keywords
PSA; Density; Prostate; Cancer; Intermediate
Introduction
Prostate cancer (CaP) constitutes a major international health problem. In Nigeria, studies have shown an increasing prevalence of the disease. [1]
The discovery of PSA has revolutionized the diagnosis of CaP however have difficulties in discriminating malignant and benign prostatic status especially in patients with grey zone of 4.0-10.0 ng/ml.
Men with PSA levels of 4.0-10.0 ng/ml fall into a ‘grey zone’ wherein only 25% of the cases are diagnosed to have cancer, while remaining 75% undergo unnecessary biopsies. [2] Hence the need for a better marker to identify this small percentage of men and prevent unnecessary biopsies. Benson et al. [3] first proposed the use of Prostate specific antigen density (PSAD) as a means of discriminating prostate cancer from the most frequent cause of PSA elevation, Benign Prostatic Hyperplasia (BPH). PSAD has been proved to be important in evaluating men with ‘grey zone’ PSA levels (4-10 ng/ml) as it helps to reduce -unnecessary biopsy and its associated complications. PSAD requires measurement of prostate volume and is expressed as PSA value divided by the prostate volume. This study aimed at determining the usefulness of PSAD among native African men with intermediate PSA of 4-10 ng/ml and establishing a cut-off value.
Research Methodology
This prospective study was conducted in the department of Urology, Jos University Teaching Hospital, Jos, Nigeria between July 2015 to August 2016 after an approval from the ethical committee of the hospital. Men with PSA of 4-10 ng/ml were recruited after informed consent.
Each subject had a comprehensive clinical evaluation involving relevant history and focused physical examination that included a digital rectal examination of the prostate gland. Each subject had serum total prostate specific antigen measured. The result was read using a microliter-well reader.
This was followed by a transabdominal ultrasound scan to determine the prostate volume using a curvilinear probe 3.5 MHz which was done by the same radiologist to avoid inter observer error. The measurement of the prostate volume was done using the ellipsoid formula- π/6 × transverse diameter × antero-posterior diameter × longitudinal diameter. [4]
The PSA density was then calculated by dividing the total PSA by prostate volume and recorded accordingly.
The subjects subsequently had digitally guided transrectal prostate biopsy. They all had prophylactic antibiotics given. A dose of intravenous ciprofloxacin 200 mg and metronidazole 500 mg were administered thirty minutes before the procedure and continued orally for five days afterwards. Caudal block was used as form of anesthesia. Prostate specimens (sextant biopsies) were taken with patient in left lateral position using a spring-loaded 18-G core needle (TRUCUT® biopsy needle) and under transrectal digital guidance. Six cores were taken from parasagittal plane halfway between the lateral border and midline of the prostate on both right and left sides from the base, mid-gland, and apex. The midline of prostate was avoided to prevent prostatic urethra injury. The specimen was stored in 10% formalin and examined histopathologically using haematoxylin-eosin stain. The histological report was recorded.
All data obtained from the study subjects were subjected to statistical analysis using the Statistical Package for Social Sciences (SPSS) version 20 ((SPSS, IBM, Chicago, IL, USA). Results were represented as tables and charts. Spearman’s rank correlation test and other appropriate test statistics were used for analysis. A p-value of <0.001 was considered statistically significant.
Results
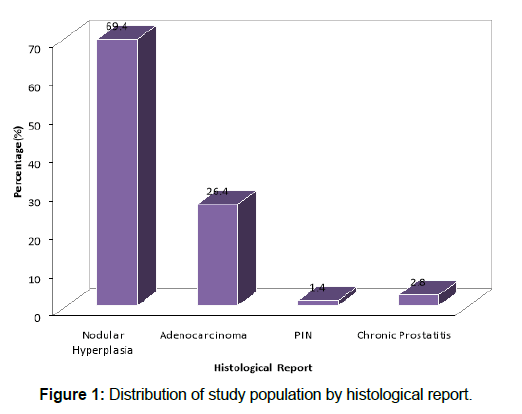
A total of 72 men who met the inclusion criteria and gave consent were recruited for the study during the period of September, 2015-March, 2017. The age range of the subjects was 47- 99 years with a mean age of 65.4 ± 10.4 years. The cancer prevalence was 26. [4] [Figure 1]. The commonest age group with cancer was 60-69 years with a mean age of 68.4 years. At a cut-off of 0.15 ng/ml2, the cancer detection rate, sensitivity and specificity of PSAD was 51.5%, 89.5% and 69.8% respectively (p <0.001) as shown in Tables 1 and 2 below. However, at cutoff of 0.12 ng/ml2, the PSAD had a sensitivity and specificity of 95.0% and 62.0% respectively with AUC 0.84 on ROC (p <0.001).
Table 1: Means of continuous variables measured.
| Variables | Mean ± S.D | Minimum | Maximum |
|---|---|---|---|
| Age (years) | 65.42 ± 10.38 | 47 | 99 |
| Prostate Volume (mls) | 63.15 ± 29.78 | 18 | 168 |
| PSA (ng/ml) | 7.27 ± 1.92 | 4 | 10 |
| PSAD (ng/ml²) | 0.14 ± 0.10 | 0.04 | 0.26 |
Table 2: Cancer detection rate using PSA density at cut-off 0.15 ng/ml².
| PSAD Test Results (ng/ml²) | Cancer | Total | Statistics | p-value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Positive (≥ 0.15) | 17 (89.5%) | 16 (30.2%) | 33 (45.8%) | Chi-Square=19.8 Kappa=0.48 |
<0.001 <0.001 |
| Negative (< 0.15) | 2 (10.5%) | 37 (69.8%) | 39 (54.2%) | ||
| Total | 19 (100.0%) | 53 (100.0%) | 72 (100.0%) | ||
Discussion
In this study, most of the patients presented in the seventh decade of life with mean age of 65.4 years. Out of these, 19 (26.4%) were diagnosed to have prostate cancer on biopsy. The mean age of those with cancer was 68.4 years. This is similar to reports from various studies which recorded the seventh decade of life as the mean age of diagnosis. [5-7]
This study showed a prostate cancer prevalence of 26.4% in men with PSA of 4 -10 ng/ml. A number of studies comparable with this finding reported 25%. [2,8] In a study by Catalona et al., [9] the prevalence rate of prostate cancer was 22% in men with an intermediate PSA level. However, a lower prevalence rate of 13.3% was reported in a similar study among patients with intermediate PSA levels by Ezenwa et al. [10] The reason given for this low yield was possibly related to the use of digital guidance for the biopsy, as against TRUS-guided biopsy used in the other studies. [11] The difference between this study and that by Ezenwa et al. [10] may be attributed to the difference in selection criteria of the study population.
In the analysis of the PSAD, the cancer patients had an average of 0.18 ng/ml2, while patients with negative results averaged 0.12 ng/ml2. Castro et al. [5] reported the cancer patients averaged 0.31 ng/ml2, while patients with negative results averaged 0.10 ng/ml2. This suggests the higher the PSAD the more likely the patient will have prostate cancer. The present study showed the sensitivity, specificity, positive predictive value and negative predictive value of PSAD to be 89.5%, 69.8%, 51.5% and 94.9% respectively. Various studies have reported different values depending on the region and cut-off used. In a similar study using a cut-off of 0.15, Djavan et al. [11] reported 83% as the sensitivity while Castro et al. [5] reported a sensitivity of 74% and specificity of 70%.
The ideal cutoff level of PSAD for detecting CaP has remained contentious in recent times. A cut-off of 0.15 ng/ml2 which has been widely used has been questioned by many scholars. This cut-off was based on data from Western patients. [12] It is documented that black men have larger prostate volume and secrete more PSA per unit tissue compared to Caucasians. [11] As such, PSAD estimation will be lower for our population. Therefore, in other to get a higher sensitivity and specificity for prostate cancer detection, a lower cut-off may be used. This was proven in this study, which revealed a higher value of sensitivity (95%) and specificity (62%) at a cut-off of 0.12 ng/ml2 (p<0.0001). This is comparable to many studies which revealed higher values of sensitivity and specificity at a lower cut-off value. Udeh et al. [13] reported the sensitivity and specificity of 95.88% and 28.7% respectively using a cut-off value of 0.04 and concluded that PSAD is useful for prostate cancer detection when this lower cut-off is used for Nigerian men. Catalona et al., [14] in a multicenter study with 773 men, suggested that the PSAD value be lowered to 0.078 ng/ml2, a value at which 95% of the tumors would be detected. Zhao et al. [15] studied 40 cases with PSA levels of 4-20 ng/ml and found that the sensitivity, specificity and PPV of PSAD at a cut-off of 0.10 ng/ml/ml was 100%, 11.1% and 22.9% respectively. Cao et al. [16] analyzed 38 patients with PSA levels of 4-10 ng/ml. They reported a sensitivity and specificity of PSAD at a cut-off of 0.13 ng/ml2 of 92.1% and 47.1% respectively and suggested that PSAD was a good predictor of prostate cancer.
A study suggested a higher cut-off in order to get a higher specificity. [17] Although, a high specificity will reduce false positive results, thereby reducing unnecessary prostate biopsy; a low sensitivity creates the problem of missing out patients with cancer which is more harmful. Thus, a balance is needed to avoid compromise either way. This study achieved this by establishing a cut-off of 0.12 which gave a sensitivity of 95% and a specificity of 62%.
The usefulness of PSAD has been proven in many studies including the present study. This study showed PSAD has a cancer detection rate of 51.5% meaning unnecessary biopsies would be avoided in approximately half of patients when PSAD is used as compared to PSA where 75% will have unnecessary biopsies. At the same time, PSAD has been shown in this study not to compromise cancer detection especially when a cut-off of 0.12 is used which gave a sensitivity of 95%. Comparative studies have shown PSAD to be the most useful variable among total PSA, PSA density and % free/total PSA. [15,17]
Conclusion
The sensitivity, specificity and positive predictive value of PSAD is 89.5%, 69.8% and 51.5% respectively at a cut-off of 0.15. It showed an improved specificity which will have an impact on the reduction of unnecessary biopsies with their consequential complications and at the same time not compromising cancer detection when used. However, at a lower cut-off of 0.12, it has a higher sensitivity (95%).
Acknowledgement
I would like to appreciate my colleagues- Drs. Audu Esla, Paul Polycarp, Jeplah Nankwat for the assistance rendered in the data collection.
My appreciation goes to my statistician, Mr. Placcid Unogwu for the data analysis and his expert guidance.
Recommendation
PSA density is useful but a reduced cut-off should be suggested for native African men because Africans have a comparatively larger prostate size compare to the Caucasians.
Conflict of Interests
There was no conflict of interest declared in this study. The conduct, results and presentation of the study were unbiased and are true reflections of the outcome of the study. All authors have unimpeded access to research facilities and the results obtained from the study were true reflections of outcome of the research.
REFERENCES
- Nwofor AM, Oranusi CK. Cancer of the prostate: Experience at Nnewi, Southeast, Nigeria. Niger J Clin Pract. 2004;7:65-68.
- Kamyar Ghabili K, Tosoian JJ, Schaeffer EM, Pavlovich CP, Golzari SE, Khajir G, et al. The History of Prostate Cancer From Antiquity: Review of Paleopathological Studies. Urology. 2016;97:8-12.
- Stephenson RA, Stanford JL. Population based prostate cancer trends in the United States: Patterns of change in the era of prostate-specific antigen. World J Urol. 1997;15:331-335.
- Ajayi I, Aremu A, Olajide A, Bello T, Olajide F, Adetiloye V. Correlation of transrectal and transabdominal ultrasound measurement of transition zone volume with post-operative enucleated adenoma volume in BPH. The Pan Afr Med J. 2013;16:149.
- Castro HAS, Iared W, Shigueoka DC, Mourão JE, Ajzen S. Contribution of PSA density in the prediction of prostate cancer in patients with PSA values between 2.6 and 10.0 ng/ml. Radiol Bras. 2011;44:205-209.
- Ajape AA, Ibrahim KO, Fakeye JA, Abiola OO. An overview of cancer of the prostate diagnosis and management in Nigeria: The experience in a Nigerian tertiary hospital. Ann Afr Med. 2010;9:113-117
- White JM JR, O'Brien DP III. Prostate Examination. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990:190.
- Ezenwa E, Tijani K, Jeje A, Ogunjimi R. Prevalence of Prostate cancer among Nigerians with intermediate total prostate specific antigen levels of 4-10 ng/ml: Experience at Lagos University Teaching Hospital, Nigeria. Int J Urol. 2012;9:1-5.
- Catalona WJ, Smith DS, Ratliff TL, Dodds KM, Coplen DE, Yuan JJ. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324:1156-1161.
- Ezenwa EV, Tijani KH, Jeje EA, Soriyan OO, Ogunjimi MA, Ojewola RW, et al. The value of percentage free prostate specific antigen (PSA) in the detection of prostate cancer among patients with intermediate levels of total PSA (4.0–10.0 ng/ml) in Nigeria. Arab J Urol. 2012;10:394-400.
- Djavan B, Remzi M, Zlotta AR, Ravery V, Hammerer P, Reissigl A, et al. Complexed prostate-specific antigen, complexed prostate-specific antigen density of total and transition zone, complexed/total prostate-specific antigen ratio, free-to-total prostate-specific antigen ratio, density of total and transition zone prostate-specific antigen: results of the prospective multicenter European trial. Urology. 2002;60:4-9.
- Sfoungaristos S, Perimenis P. Evaluating PSA Density as a predictor of biochemical failure after radical prostatectomy: Results of a prospective study after a median follow-up of 36 months. Int Scholarly research notices articles. 2013;1-5.
- Udeh EI, Nnabugwu II, Ozoemena FO, Ugwumba FO, Aderibigbe ASO, Ohay SR, et al. Prostate-specific antigen density values among patients with symptomatic prostatic enlargement in Nigeria. World J Surg Onc. 2016;14:1-7.
- Catalona WJ, Southwick PC, Slawin KM, Partin AW, Brawer MK, Flanigan RC, et al. Comparison of percent free PSA, PSA density, and age-specific PSA cutoffs for prostate cancer detection and staging. Urology. 2000;56:255-260.
- Cao XL, Gao JP, Han G, Tang J, Hong BF. Relationship between screening by stratifying cases into groups on prostate specific antigen level and the positive rate of transrectal ultrasound guided systematic sextant prostate biopsy. Zhonghua Wai Ke Za Zhi 2006; 44:372-375.
- Mohammed AZ, Edino ST, Ochicha O, Gwarzo AK, Samaila AA. Cancer in Nigeria: A 10-year analysis of the Kano Cancer Registry. Niger J Med. 2008;17:280-284.
- Sasaki R, Habuchi T, Sato K, Akao T, Kakinuma H, Zhang LQ, et al. The clinical utility of measuring total PSA, PSA Density, γ-seminoprotein and γ-seminoprotein/total PSA in Prostate Cancer Prediction. Jpn J Clin Oncol 2000;30:337-342.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.