Wasting of Extensor Digitorum Brevis as a Decisive Preoperative Clinical Indicator of Lumbar Canal Stenosis: A Single‑center Prospective Cohort Study
- *Corresponding Author:
- Dr. Munakomi S Department of Neurosurgery, International Society for Medical Education, Chitwan - 23, Nepal. E-mail: sunilmunakomi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: The dilemma in managing patients with low back ache lies in differentiating radiculopathy from lumbar canal stenosis. This has a huge bearing in patients being planned for surgical intervention as underperforming leads to failed back syndrome whereas over‑doing leads to instability. There still remains a loophole in clinically diagnosing lumbar canal stenosis. Aim: We opt to utilize a simple bedside clinical examination in routinely assessing patients presenting with low back ache in ruling out underlying canal stenosis. Subjects and Methods: We performed a prospective study on 120 consecutive patients presenting with low back ache in the spine clinic. Each of them was neurologically examined and thoroughly assessed for wasting of extensor digitorum brevis (EDB) muscles. These were then correlated with the radio‑imaging and the intraoperative findings. Results: Lumbar canal stenosis was mostly observed in the age group of 50–60 years. Diagnosis for L3/4 canal stenosis was made in 44/120 (36.6%), L5‑S1 in 52/120 (43.3%), and L3/L4/L5 level in 48/120 (40%) of patients. EDB wasting was seen unilaterally in 72/120 (60%) and bilaterally in 36/120 (30%) of the study group. Conclusion: This study appraises the clinical implication of observing for the wasting of EDB muscle so as to aid in the diagnosis of lumbar canal stenosis. This simple bedside clinical pearl can help us in predicting the need of further imaging studies and also in taking right therapeutic decision.
Keywords
Extensor digitorum brevis, Lumbar canal, Stenosis
Introduction
Degenerative lumbar spinal stenosis describes a condition in which there is diminished space available for the neural and vascular elements in the lumbar spine. Mostly, it is secondary to degenerative changes in the spinal canal. Patients mostly present with a history of gluteal or lower extremity symptoms exacerbated by walking or standing but characteristically improve or resolve with sitting or bending forward. Patients whose pain is not made worse with walking have a low likelihood of stenosis.[1] Till date, radio-images have been the gold standard in ruling out canal stenosis. However, expensive radiological armamentarium may not be an answer in screening every patient presenting with a low back ache for ruling out canal stenosis. There still is the missing link in the clinical diagnosis of this global health issue.
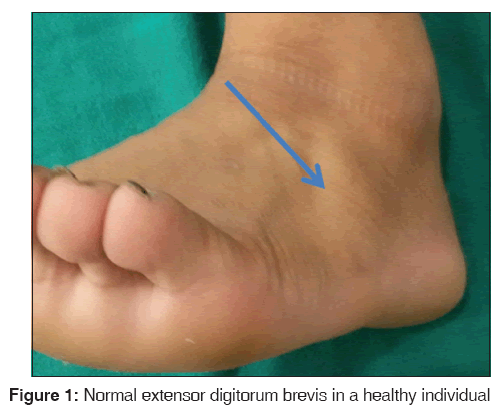
The extensor digitorum brevis (EDB) muscle arises from the distal part of the superolateral surface of the calcaneus [Figure 1].
It runs distally across the dorsum of the foot and finally divides into four slips.[2] Medial slip inserts onto the base of the proximal phalanx of the great toe. The other slips attach to the lateral sides of the tendons of the extensor digitorum longus for the second, third, and fourth toe.
Wasting of EDB has been taken as a marker for L5/S1 radiculopathy.[3,4] Herein, we highlight the clinical importance of observing for evidence of EDB wasting as a marker for underlying lumbar canal stenosis. This simple bedside clinical observation can help us make correct surgical strategy and thereby prevent failed back syndrome by carrying out decompressive laminectomy rather than just tackling the disc in such groups.
Subjects and Methods
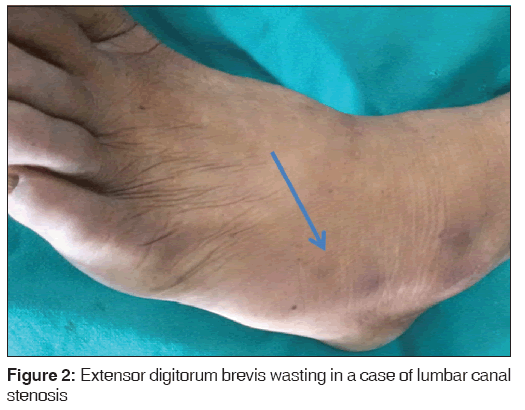
We included 120 consecutive patients presenting to the spine clinic in the Department of Neurosurgery, College of Medical Sciences, with a complaint of low back ache from January 2012 to January 2013. They were clinico-radiologically assessed for features of radiculopathy and canal stenosis. Only the trained residents in the spine team assessed for the presence of EDB wasting in all the patients [Figure 2] and were counterchecked by the consultants so as to decrease the inter-rater variability. We compared the bulk of the muscle of the patients with their healthy counterparts of the same sex and age group so as to minimize the confounding bias due to age-related and chronic illnesses related atrophy in the muscle. To minimize the intra-rater variability, whenever in doubt, we advocated the use of ultrasound scan to assess and compare the bulk of the muscle. Whenever possible, we recommend electromyography study along with motor conduction velocity so as to confirm the same.
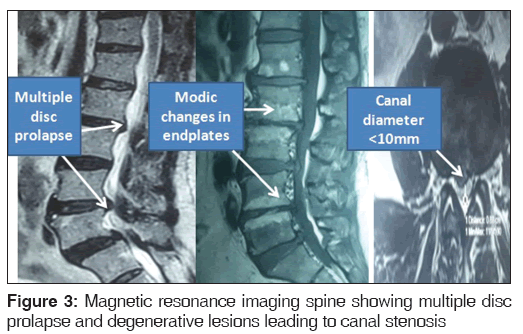
Magnetic resonance imaging (MRI) study guideline included getting a thin (4–5 mm) MRI sections with a combination of T1 and T2 pulse sequences in both axial and sagittal planes with additional angled and stacked axial sections. Anteroposterior diameter (<10 mm) [Figure 3] and cross-sectional area (<70 mm) of spinal canal and MRI finding of positive sedimentation sign were taken into account for diagnosing canal stenosis.
We also studied dynamic X-ray spine to see for any instability. In the presence of instability based on Posner’s criteria, patients were offered decompression with fusion if the stenosis was moderate to severe. We also stressed on the need of standing full-length lateral radiographs of the spine to check for sagittal balance of the patients which has a bearing of increasing instability after performing procedures such as laminectomy.
Most of the patients were mobilized early from the next morning of the day of surgery. Postoperative X-ray lumbosacral spine was taken for groups undergoing hemilaminectomy and decompressive laminectomy so as to rule out spinal instability. Most of the patients were discharged within 72 h of surgery. Improvement in the muscle groups and the improvement in the wasting of the muscles were routinely assessed for 1 year in the outpatient department.
This study was approved by the Educational Ethical Board of College of Medical Sciences. Both oral and written consent were taken from all the patients included in the study.
Results
Clinical profile
On average, the participating patients were 56-year-old (standard deviation [SD] 14.0; age range: 20–88 years). Mean age for lumbar canal stenosis was 56.30 (13.95) (mean: Years [SD]). Male to female ratio was 1.5:1. Mean age for intervertebral disc prolapse (IVDP) in our study group was 27 years (age range from 19 to 46 years). In this study, group ratio of canal stenosis and disc prolapsed was 60:40 among males and 40:60 among females, respectively.
Clinical findings
EDB wasting was observed unilaterally in 72/120 (60%) and bilaterally in 36/120 (30%). Calf muscle wasting was seen unilaterally in 36/120 (30%) bilaterally in 18/120 (15%). Likewise, weakness of extensor hallusus longus (EHL) was seen in 76/120 (63.3%), dorsalis flexors (DF) in 100/120 (83.3%), plantar flexors (PF) in 44/120 (36.6%), and knee flexors (KF) in 66/120 (55%), respectively.
Radiological investigations
L4–l5/L5-S1 IVDP was observed in 40/120 (33.3%), L4–L5/L5-S1 IVDP and canal stenosis was seen in 44/120 (36.6%) and canal stenosis alone was observed in 36/120 (30%) of patients.
Preoperative canal stenosis
Diagnosis for L3/L4 canal stenosis was made in 44/120 (36.6%), L5/S1 in 52/120 (43.3%), and L3/L4/L5 level in 48/120 (40%) of patients.
Per operative intervertebral disc prolapse
Intraoperatively, axillary variant of disc was seen in 16/120 (13.3%) and shoulder variant in 8/120 (6.6%) of patients. Pure disc entity was observed in 12/120 (10%) whereas the combination of disc and canal stenosis was observed in 12/120 (10%).
Morbidity among patients
The incidental durotomy in our study was seen in 8/120 (6.6%) of cases. Likewise, postoperative cerebrospinal fluid (CSF) leak was seen in 2/120 (1.6%), discitis in 2/120 (1.6%), and pseudomeningocele occurred in 2/120 (1.6%) of patients.
Follow-up of patients
During follow-up of our patients, no neurological deficits were seen in 114/120 (95%) of patients. Weakness of DF/EHL weakness persisted among 6/120 (5%) of patients. At 2 years of follow-up, unilateral EDB wasting was seen in only 38/120 (31.6%) of patients compared to 72/120 (60%) preoperatively. Bilateral EDB wasting persisted in 22/120 (18.3%) of patients compared to 36/120 (30%) preoperatively.
Discussion
With the increasing longevity a continually climbing proportion of middle-aged and elderly persons, low back ache is surely going to be a ubiquitous and disabling disease of humankind.[5] Lumbar canal stenosis has a significant negative impact to the quality of life in such subset of population.[6]
Most of these patients present with features of intermittent neurological claudication.[7] The main dilemma in managing such patients lies in differentiating true disc disease from associated canal stenosis secondary to degenerative changes.
The diagnosis of the spinal stenosis is aided by the radiological studies.[8,9] Computerized tomogram of lumbar spine shows characteristics trefoil appearance of the canal. In the MRI of the spine, there is loss of CSF surrounding the canal. Guideline suggests getting a thin (4–5 mm) MRI sections with a combination of T1, proton density, and T2 pulse sequences in both axial and sagittal planes with additional angled and stacked axial sections.[1] Meta-analysis has shown the sensitivity of MRI in the diagnosis of adult spinal stenosis to be 81%–97%, of computed tomography 70%–100% and myelography 67%–78%.[10] Besides the anteroposterior diameter (<10 mm) and cross-sectional area (<70 mm) of spinal canal, MRI finding of positive sedimentation sign is a good positive sign to rule in lumbar spinal stenosis with high specificity and sensitivity.[11,12] Lumbar canal stenosis was mostly observed in the age group of 50–60 years. Diagnosis for L3–L4 canal stenosis was made in 44/120 (36.6%), L5/S1 in 52/120 (43.3%), and L3/L4/L5 level in 48/120 (40%) of patients in our study group.
However, in the developing countries like ours, the financial aspect of the patients and the limitations of resources in many hospitals may play a pivotal role in limiting ourselves to clinical diagnosis.
The management aspects of lumbar disc disease range from conservative, epidural steroids injection, minimally invasive approaches to decompressive laminectomies.[13-17] However, failure to correctly diagnose and then treat the canal stenosis may invariably lead to failed back syndrome in the patients.[18]
Preservation of the posterior elements is the most important factor in the success of decompression surgery for lumbar canal stenosis, but the occurrence of postoperative instability and restenosis has been a shortcoming of laminectomy.[19,20] Despite affording a wide decompression, laminectomy can result in segmental instability and paravertebral muscle atrophy.[21] Fenestration has been developed to solve this problem of laminectomy, but there is limited access and insufficient decompression in the lateral recesses and added risk for neural injury in a small working space.[22,23]
There is also need of dynamic X-ray study to see for any instability. In the presence of instability based on Posner’s criteria, the patient should be offered decompression with fusion if the stenosis is moderate to severe.[1] In particular, three measures are of vital importance (1) global sagittal balance (C7 plumb line [C7PL], C7/sacro-femoral distance ratio and spino-sacral angle), (2) spinopelvic morphology (pelvic incidence, sacral slope, and pelvic tilt), and (3) spinal parameters (lumbar lordosis and thoracic kyphosis). Jeon et al. have found posterior migration of the C7PL and increase lumbar lordosis following decompressive laminectomy, in their evaluation of 40 patients over 2 years.[24]
In the one hand, under-doing can lead to failed back syndrome, and on the other hand, over-doing leads to instability.
Therefore, simple assessment of the bulk of the EDB muscle on both sides can predict the underlying canal stenosis and thereafter help make correct therapeutic decisions. EDB wasting was seen unilaterally in 72/120 (60%) and bilaterally in 36/120 (30%) of the study group.
EDB being a muscle with the smallest bulk in foot is clinically very sensitive for L5 radiculopathy. There are earlier reports in cases of spina bifida or tethered cord syndrome where late manifestation has led to EDB weakness.[25]
However, North American Spine Society in their recommendation have found insufficient evidence to make a recommendation for or against certain physical findings for the diagnosis of degenerative lumbar spinal stenosis including an abnormal Romberg test, thigh pain exacerbated with extension, sensorimotor deficits, leg cramps, and abnormal Achilles tendon reflexes.[1]
There is a pivotal need of comprehensive clinical evaluation of spine and neurological function before embarking on surgical management of low back ache or radiculopathy. This is becoming ever vital as the incidence of failed back syndrome is on the rise, a major causative factor being an incomplete clinical evaluation of the patient.[18]
The positive aspects of our study are the observation for the EDB wasting by the members of the spine team only so as to reduce the interobserver bias in the study. We had also blinded the clinical examiner of the radiological findings and conducted a prospective study so as to limit the post hoc effect.
The limitation of the study is the learning curve in assessing the wasting of the EDB muscle. This can be limited by the adjunct use of ultrasound in assessing the bulk of the muscle and comparing to the healthy volunteer of the same age group. We can also utilize nerve conduction tests on the muscles. Furthermore, multicentric randomized control trials with larger inclusion of study group will surely help us reach further conclusions on this verdict.
Conclusion
Focal canal stenosis revealed isolated marked wasting of EDB in addition to EHL/DF/PF/KF weakness. Pure disc prolapsed on the contrary revealed EHL/DF/PF/KF weakness without wasting. EDB wasting is a decisive clinical indicator of significant canal stenosis as opposed to pure disc prolapsed. In the era of micro- and endoscopic procedures, this assumes importance for planning the type of procedure and a word of caution for the novices in the vast realms of lumbar spine procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Watters WC 3rd, Baisden J, Gilbert TJ, Kreiner S, Resnick DK, Bono CM, et al. Degenerative lumbar spinal stenosis: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J 2008;8:305-10.
- Sirasanagandla SR, Swamy RS, Nayak SB, Somayaji NS, Rao MK, Bhat KM. Analysis of the morphometry and variations in the extensor digitorum brevis muscle: An anatomic guide for muscle flap and tendon transfer surgical dissection. Anat Cell Biol 2013;46:198-202.
- Sinanovic O, Custovic N. Musculus extensor digitorum brevis is clinical and electrophysiological marker for L5/S1 radicular lesions. Med Arh 2010;64:223-4.
- Kelly PM, Byrne S, Fleming P, Mullett H, Shagu T, Dowling F. Wasting of the extensor digitorum brevis – A reliable sign of l5 radiculopathy. A prospective study. J Bone Joint Surg Br 2004;86-B Suppl II: 121.
- Humphreys SC, Eck JC. Clinical evaluation and treatment options for herniated lumbar disc. Am Fam Physician 1999;59:575-82, 587-8.
- Otani K, Kikuchi S, Yabuki S, Igarashi T, Nikaido T, Watanabe K, et al. Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: An epidemiological cross-sectional study of 1862 community-dwelling individuals. ScientificWorldJournal 2013;2013:590652.
- Kobayashi S. Pathophysiology, diagnosis and treatment of intermittent claudication in patients with lumbar canal stenosis. World J Orthop 2014;5:134-45.
- Modic MT, Masaryk T, Boumphrey F, Goormastic M, Bell G. Lumbar herniated disk disease and canal stenosis: Prospective evaluation by surface coil MR, CT, and myelography. AJR Am J Roentgenol 1986;147:757-65.
- Steurer J, Roner S, Gnannt R, Hodler J; LumbSten Research Collaboration. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: A systematic literature review. BMC Musculoskelet Disord 2011;12:175.
- Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur Spine J 2011;20:513-22.
- Mobaleghi J, Allahdini F, Nasseri K, Ahsan B, Shami S, Faizi M, et al. Comparing the effects of epidural methylprednisoloneacetate injected in patients with pain due to lumbar spinal stenosis or herniated disks: A prospective study. Int J Gen Med 2011;4:875-8.
- Dawood OM, Hassan TA, Mohey N. The MRI finding of the nerve root sedimentation sign: Its clinical validity and operative relativity for patients with lumbar spinal stenosis. Egypt J Radiol Nucl Med 2014;45:203-9.
- Kent DL, Haynor DR, Larson EB, Deyo RA. Diagnosis of lumbar spinal stenosis in adults: A metaanalysis of the accuracy of CT, MR, and myelography. AJR Am J Roentgenol 1992;158:1135-44.
- Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res 2015;473:1940-56.
- Wong AP, Smith ZA, Lall RR, Bresnahan LE, Fessler RG. The microendoscopic decompression of lumbar stenosis: A review of the current literature and clinical results. Minim Invasive Surg 2012;2012:325095.
- Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine (Phila Pa 1976) 1992;17:1-8.
- Thomas NW, Rea GL, Pikul BK, Mervis LJ, Irsik R, McGregor JM. Quantitative outcome and radiographic comparisons between laminectomy and laminotomy in the treatment of acquired lumbar stenosis. Neurosurgery 1997;41:567-74.
- Long DM. Failed back surgery syndrome. Neurosurg Clin N Am 1991;2:899-919.
- Sangwan SS, Aggarwal S, Mittal R, Kundu ZS, Siwach RC. Easy and economical alternative to the relton-hall frame for posterior spinal surgeries. J Orthop Surg (Hong Kong) 2003;7:139-41.
- Robertson PA, Grobler LJ, Novotny JE, Katz JN. Postoperative spondylolisthesis at L4-5. The role of facet joint morphology. Spine (Phila Pa 1976) 1993;18:1483-90.
- Bresnahan L, Ogden AT, Natarajan RN, Fessler RG. A biomechanical evaluation of graded posterior element removal for treatment of lumbar stenosis: Comparison of a minimally invasive approach with two standard laminectomy techniques. Spine (Phila Pa 1976) 2009;34:17-23.
- Young S, Veerapen R, O’Laoire SA. Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: Preliminary report. Neurosurgery 1988;23:628-33.
- Benz RJ, Garfin SR. Current techniques of decompression of the lumbar spine. Clin Orthop Relat Res 2001; 384:75-81.
- Jeon CH, Lee HD, Lee YS, Seo HS, Chung NS. Change in sagittal profiles after decompressive laminectomy in patients with lumbar spinal canal stenosis: A 2-year preliminary report. Spine (Phila Pa 1976) 2015;40:E279-85.
- Macnicol MF, Nadeem RD. Evaluation of the deformity in club foot by somatosensory evoked potentials. J Bone Joint Surg Br 2000;82:731-5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.