Outcomes of Vacuum-Assisted Closure versus Conventional Dressings in Patients with Diabetic Foot Ulcers
Received: 19-Aug-2024, Manuscript No. AMHSR-24-145814; Editor assigned: 21-Aug-2024, Pre QC No. AMHSR-24-145814 (PQ); Reviewed: 04-Sep-2024 QC No. AMHSR-24-145814; Revised: 13-Aug-2025, Manuscript No. AMHSR-24-145814 (R); Published: 20-Aug-2025
Citation: Ranjan P, et al. Outcomes of Vacuum-Assisted Closure versus Conventional Dressings in Patients with Diabetic Foot Ulcers. Ann Med Health Sci Res. 2025;15:1-11
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: To compare the effectiveness of a Vacuum-Assisted Closure (VAC) dressing to that of conventional dressing in patients with diabetic foot ulcers. In view of this, the present study was planned to compare Vacuum Assisted Closure (VAC) and conventional dressing methods for diabetic foot ulcers in terms of the rate of granulation tissue formation, bacterial clearance at the end of therapy and duration of wound healing.
Materials and methods: This was a randomized comparative study conducted in the Department of General Surgery, Indira Gandhi Institute of Medical Sciences, Patna, from January 21 to December 22.50 patients with lower limb diabetic ulcers were included; these patients were randomized into two groups. Conventional dressing was performed (n=31), and Vacuum Assisted Enclosure (VAC) dressing was used (n=19). Patient outcomes were compared after dressing. All the statistical analyses were performed with SPSS software, and a P-value<0.05 was used to indicate statistical significance.
Results: Compared to those in the conventional dressing group, the Vacuum Assisted Closure (VAC) dressing group was comparable in terms of age, sex and associated comorbidities (p-value>0.05); took less but comparable amounts of granulation tissue to appear (6.94 ± 2.61 vs. 9.03 ± 2.30, p value=0.29); took a signi icantly shorter duration for wound culture to be negative (11.36 ± 4.47 vs. 14.83 ± 3.89, p value=0.037); and took a significantly shorter duration for wound healing (36.84 ± 9.34 vs. 43.16 ± 9.22, p value=0.033).
Conclusion: Vacuum-Assisted Closure (VAC) dressing was advantageous over conventional dressing for the dressing of lower limb diabetic ulcers in terms of the time taken for the formation of granulation tissue, the time taken for wound culture to be negative and long-term follow-up, and the duration of wound healing. Vacuum Assisted Closure (VAC) dressing for chronic wounds or ulcers seems to be a promising option compared with conventional dressing, and the short-term results are good.
Keywords
Diabetic ulcer, Vacuum dressing, Normal saline dressing, Lower limb
Introduction
In India, one of the first nation’s most commonly affected by diabetes, foot ulceration is the most common complication, affecting approximately 15% of diabetic patients [1]. Patients with DM have up to a 25-35% lifetime risk of developing a foot ulcer [2], which precedes amputation in up to 85% of cases [3]. The management of diabetic foot ulcers is largely determined by their severity (grade), vascularity, and presence of infection [4-6]. The optimal topical therapy for diabetic foot ulcers is not well defined. Saline moistened gauze has been the standard method; however, it has been difficult to maintain a moist wound environment continuously. Subsequently, various hydrocolloid wound gels, growth factors, enzymatic debridement compounds, hyperbaric oxygen therapy, cultured skin substitutes, and other wound therapies have been advocated [7]. Negative-Pressure Wound Therapy (NPWT) is a relatively newer technique for managing complex wounds. It was first described by Charikar [8] as an experimental technique for treating subcutaneous fistulas. However, the clinical work of Argenta and Moryk was a decade later and allowed Negative-Pressure Wound Therapy (NPWT) to be recognized as a useful clinical tool for managing complex and difficult wounds [9-11]. Currently, Negative-Pressure Wound Therapy (NPWT) is well established for treating traumatic wounds, general surgical wounds, and diabetic foot wounds. Supporting evidence for the use of Negative-Pressure Wound Therapy (NPWT) in the treatment of diabetic foot wounds includes numerous prospective and multicenter randomized controlled trials [12]. Vacuum Assisted Closure (VAC) is a noninvasive, active wound management system that uses negative pressure to enhance the healing process, increase local blood flow, reduce edema and bacterial colonization and promote closure of the wound by promoting the rapid formation of granulation tissue [13]. Recent studies have shown that the application of sub-atmospheric pressure to the wound site in a controlled manner has an important role in assisting wound healing [14]. Complex effects at the woundâ??dressing interface following the application of a controlled vacuum force have been documented. These include changes at the microscopic, molecular and macroscopic levels; at the tissue level, interstitial fluid flow and exudate management; edema reduction; and effects on wound perfusion, protease profiles, growth factor and cytokine expression and cellular activity, all of which lead to enhanced granulation tissue formation and improved wound healing parameters [15-17]. In view of this, the present study was planned to compare Vacuum Assisted Closure (VAC) and conventional dressing methods for diabetic foot ulcers in terms of the rate of granulation tissue formation, bacterial clearance at the end of therapy and duration of wound healing.
Materials and Methods
The study was conducted in the Department of General Surgery, IGIMS Patna, Bihar, India, after obtaining clearance from the Institutional Ethics Committee (IEC). Informed written consent was obtained from each patient. This was a prospective single-center, randomized comparative study comparing two methods for treating diabetic foot ulcer dressings. The study was carried out from December 2020 to December 2022.
Inclusion criteria
• Above 18 years of age.
• Informed written consent will be obtained from the patient.
• Patients with lower limb ulcers with ulcer sizes between 5 and 15 cm.
• Patients who are able and willing to comply with the study procedure.
Exclusion criteria
• Patients aged >70 years.
• Pregnant or nursing mothers.
• People on medications, such as corticosteroids, immunosuppressive agents or chemotherapy.
• Patients with underlying osteomyelitis of the bone.
• Patients not willing to participate in the study.
Sample size
A sample of 50 patients was included in the study. Eligible patients were informed about the study by the attending doctor at the outpatient Department of General Surgery.
The patient was seen in the Surgery Outpatient Department (OPD). A history was taken, and a clinical examination was performed. The patients who fulfilled the inclusion criteria were given the consent form to sign, and after providing consent for their participation in the study, they were included in the participation pool. The total participating pool was divided randomly into 2 groups.
Methods
Wounds of all the patients included in the study underwent surgical debridement initially and during subsequent dressing changes to remove necrotic tissue and slough. Patients in both groups were administered insulin therapy according to their blood sugar levels, and injectable antibiotics were started empirically initially and then according to the culture and sensitivity reports. Patients admitted with other comorbidities, such as hypertension, tuberculosis, and hypothyroidism, were treated per the consultation provided by the respective departments of the institute; if any intervention was needed, the patient was free to undergo the intervention.
Group A (vacuum-assisted closure): After debridement in the emergency operation theater, a foam-based dressing was applied to the wounds of the patients in the study group under aseptic conditions. The dressing was covered with an adhesive drape to create an airtight seal. An evacuation tube embedded in the foam was connected to a vacuum, and subatmospheric (negative) pressure was applied within a range of 80-125 mmHg on a continuous basis for 96 hours. The tube drained the secretion into a collection canister. In this way, a previously opened wound was converted into a controlled, closed and moist wound. Dressings were regularly changed every 4 days during the admission period.
Group B (conventional dressing): Patients were treated with conventional dressings. Alternate day dressings were applied during the admission period.
Wound tracing and photos were taken every 4 days during the first two weeks after admission to look for granulation tissue and compare the wound size. A swab was taken for culture at admission and every fourth day during the first two weeks after admission. On the 8th day, culture sensitivity, wound size, and granulation tissue were noted. Ulcers were treated until the wound was closed spontaneously or surgically or until completion of the 8-week period, whichever occurred earlier. Patients who were discharged from the hospital after wound closure were followed monthly via the surgical OPD. Treatment success was defined as wound closure within a period of 8 weeks, and failure was defined as the inability to achieve wound closure within 8 weeks.
Statistical analysis
Categorical variables are presented as numbers and percentages, and continuous variables are presented as the mean ± SD and median. The normality of the data was tested by the Kolmogorovâ??Smirnov test. If the assumption of normality was rejected, then a nonparametric test was used. The statistical tests will be applied as follows. Quantitative variables were compared between the two groups using the unpaired t test or Mannâ??Whitney test (when the data sets were not normally distributed). Qualitative variables were compared using the Chi-square test or Fisher’s exact test. A p value of <0.05 was considered to indicate statistical significance. The data were entered into the MS Excel spreadsheet, and analysis was performed using Statistical Package for Social Sciences (SPSS) version 22.0.
Computerized randomization technique-To randomly select between two groups, the random number generating function RANDBETWEEN () was used, with the lower limit set to 1 and the upper limit set to 2. If 1 was generated, the conventional dressing group was allocated, and if 2 was generated, the Vacuum Assisted Closure (VAC) dressing group was allocated (Figure 1).
Figure 1: Application of Vacuum-Assisted Closure (VAC) dressing on day 1.
Results
The demographic details of the patients in our study are provided in Tables 1-4. The overall mean age of the patients in the conventional dressing group was 51.7097 years, whereas that of the Vacuum Assisted Closure (VAC) group was 52.9474 years. Thirty-eight patients were males, and 18 were females.13 Patients had hypertension associated with type 2 diabetes, whereas only 3 patients had associated hypothyroidism.
| Age in group | Conventional dressing | Vacuum-Assisted Closure (VAC) | Total |
| ≤ 40 | 2 | 2 | 4 |
| 41-50 | 14 | 6 | 20 |
| 51-60 | 10 | 6 | 16 |
| 61-70 | 5 | 5 | 10 |
| Total | 31 | 19 | 50 |
| Note: Chi-square value: 1.4007; p value: 0.7054 | |||
Table 1: Association between age in group: Type of dressing used.
| Type of dressing used | |||
| Gender | Conventional dressing | Vacuum-Assisted Closure (VAC) | Total |
| Female | 9 | 3 | 12 |
| Male | 22 | 16 | 38 |
| Total | 31 | 19 | 50 |
| Note: Chi-square value: 1.1326; p value: 0.2872 Odds ratio: 2.1818 (0.5084, 9.3643) |
|||
Table 2: Association between gender and type of dressing used.
| Type of dressing used | |||
| Comorbidity | Conventional dressing | Vacuum-Assisted Closure (VAC) | Total |
| T2DM | 22 | 10 | 32 |
| T2DM, HTN | 7 | 6 | 13 |
| T2DM, TB | 0 | 2 | 2 |
| T2DM,Thyroid | 2 | 1 | 3 |
| Total | 31 | 19 | 50 |
| Note: Chi-square value: 4.2766; p value: 0.2331 T2DM: Type 2 Diabetes Mellitus; HTN: Hypertension; TB: Tuberculosis |
|||
Table 3: Association between comorbidity and type of dressing used.
| Number | Mean | SD | Minimum | Maximum | Median | p value | ||
| Age | Conventional dressing | 31 | 51.7097 | 8.415 | 39 | 70 | 50 | 0.6205 |
| Vacuum-assisted closure | 19 | 52.9474 | 8.7017 | 38 | 66 | 52 |
Table 4: Distribution of mean age: Type of dressing used.
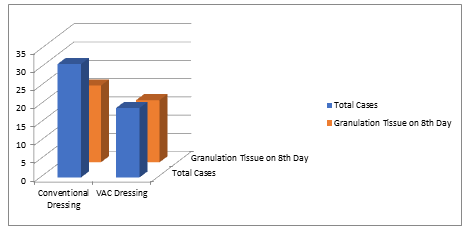
In this study, 21 out of the 31 patients in the conventional dressing group developed granulation tissue at the end of the 8 th day, whereas 17 out of the 19 patients in the Vacuum Assisted Closure (VAC) dressing group had granulation tissue at the end of the 8th day (Figure 2).
The mean ± SD of time taken for granulation tissue to appear (days) in the conventional dressing group was 9.03 ± 2.30, which was comparable to that in the vacuum-assisted closure group (6.94 ± 2.61) (p value=0.292). The results are shown in Table 5.
Figure 2: Chart comparing the appearance of granulation tissue on the 8th day after dressing.
| Number | Mean | SD | Minimum | Maximum | Median | p value | ||
| Time taken for granulation tissue to appear (Days) | Conventional dressing | 31 | 9.0322 | 2.3019 | 4 | 12 | 8 | 0.292 |
| Vacuum-assisted closure | 19 | 6.9473 | 2.6135 | 4 | 12 | 8 |
Table 5: Distribution of the mean time taken for granulation tissue to appear (days): Type of dressing used.
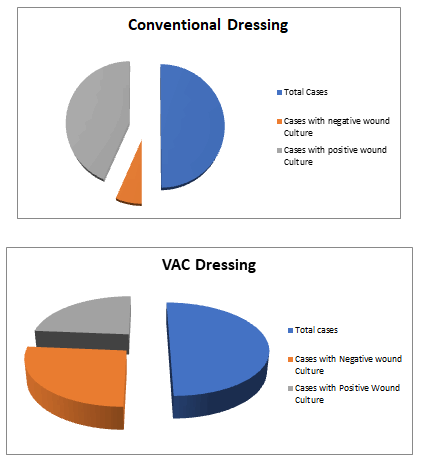
In the present study, which was performed at the end of the 8 th day, sterile wound cultures were obtained for only 4 out of the 31 patients in the conventional dressing group, whereas Ranjan P, et al.: Outcomes of Vacuum-Assisted Closure versus Conventional Dressings in Patients with Diabetic Foot Ulcers 4 Annals of Medical and Health Sciences Research | Volume 15 | Issue 4 | July 2025 Table 3: Association between comorbidity and type of dressing used. sterile wound cultures were obtained for 10 out of the 19 patients in the Vacuum Assisted Closure (VAC) dressing group (Figure 3).
Figure 3: Charts comparing sterile wound culture on the 8th day after dressing.
The mean ± SD of time taken for wound culture to be negative (days) in the conventional dressing group was 14.83 ± 3.89, which was significantly greater than that in the vacuum assisted closure group (11.37 ± 4.47) (p value=0.037). The results are shown in Table 6.
| Number | Mean | SD | Minimum | Maximum | Median | p value | ||
| Time taken for wound culture to be negative (days) | Conventional dressing | 31 | 14.8387 | 3.8909 | 4 | 20 | 14 | 0.037 |
| Vacuum-assisted closure | 19 | 11.3684 | 4.4747 | 4 | 20 | 14 |
Table 6: Distribution of the mean time taken for wound culture to be negative (days): A type of dressing used.
The mean ± SD of the duration of healing in conventional dressing was 43.17 ± 9.22, which was significantly greater than that in vacuum-assisted closure dressing (36.84 ± 9.34). (p value=0.033). The results are shown in Table 7.
| Number | Mean | SD | Minimum | Maximum | Median | p value | ||
| Duration of healing (days) | Conventional dressing | 31 | 43.1612 | 9.2271 | 28 | 62 | 42 | 0.033 |
| Vacuum-assisted closure | 19 | 36.8421 | 9.3408 | 18 | 58 | 40 |
Table 7: Distribution of the mean duration of healing (days): Type of used dressing.
Discussion
The present study was a randomized comparative study of 50 known diabetic patients with lower limb ulcers (31 patients who underwent conventional dressing and 19 patients who underwent Vacuum Assisted Closure (VAC) dressing); we aimed to compare the effectiveness of conventional dressing with Vacuum Assisted Closure (VAC) in patients with lower limb diabetic ulcers. We found that Vacuum-Assisted Closure (VAC) dressing shortened the duration needed for granulation tissue to appear, decreased the duration needed for wound culture to become negative and decreased the duration needed for healing. The study demographics of the population showed that the cases were comparable to the controls in terms of age, sex and associated comorbidities. In a randomized comparative trial such as ours, the similarity of patient characteristics ensures that any difference in outcome is purely due to intervention and not due to chance bias. In our study, most of the patients usually presented with chronic nonhealing lower limb ulcers due to the chronicity of the disease (T2DM) associated with other comorbidities. Our study consisted of 50 patients who were randomly divided into two groups: Group A, composed of 31 patients who underwent conventional dressing; and group B, composed of 19 patients who underwent Vacuum-Assisted Closure (VAC) dressing. Among other studies, Lone et al. studied 56 patients who were randomly divided into two even groups [7]. The management of foot ulcers is largely determined by the grade of the ulcer, the vascularity, and the presence of infection. Current therapeutic options for diabetic foot ulcer management include repeated debridement, pressure offloading, ischemia treatment, metabolic stabilization and preventive strategies incorporated at the primary healthcare level. Several studies have shown that, compared with moisturized saline gauze, Negative-Pressure Wound Therapy (NPWT) is associated with faster healing. Vacuum-Assisted Closure (VAC) is generally well tolerated and, with few contraindications or complications, is quickly becoming a mainstay of current wound care. Hence, we planned to use Negative-Pressure Wound Therapy (NPWT) for the treatment and rapid healing of diabetic foot ulcers. Duration for granulation tissue to appear in the present study, compared to those in the conventional dressing group, the VacuumAssisted Closure (VAC) group took less but comparable amounts of granulation tissue to appear (9.032 ± 2.30 vs. 6.94± 2.61, p value-0.29). Among previous studies, Lone et al. reported that, compared with patients in the conventional dressing group, patients in the Vacuum-Assisted Closure (VAC) group took significantly less time for granulation tissue to appear (66.7% of Vacuum-Assisted Closure (VAC) group patients developed granulation tissue by the end of 4 weeks vs. 28% of patients in the case of conventional dressing) (p value=0.049) [7]. In D'Souza et al., at the end of the first dressing on day 4, approximately 70% of wounds in the Vacuum-Assisted Closure (VAC) group had red granulation tissue, whereas 47% of those in the conventional dressing group had significantly more granulation tissue (p value=0.038) [1]. In the present study, compared to those in the conventional dressing group, the duration of wound culture negativity was significantly shorter in the VacuumAssisted Closure (VAC) group (11.37 ± 4.47 vs. 14.83 ± 3.89, p value-0.037). Among previous studies, Lone et al. reported that, compared with those in week 2, the cultures in week 1 itself were sterile after the application of Vacuum-Assisted Closure (VAC) in normal dressing [7]. However, in D’Souza et al., in the Vacuum-Assisted Closure (VAC) group, 72.73% of ulcers had no bacteria at the end of therapy, whereas in the conventional dressing group, 79.17% were rendered sterile at the end of therapy (duration of therapy-2 weeks) [1]. Duration of Wound Healing In the present study, compared to those in the conventional dressing group, the VacuumAssisted Closure (VAC) group had a significantly shorter duration of wound healing (36.84 ± 9.34 vs. 43.17 ± 9.22, p value=0.033). According to previous studies, in Lone et al., the majority of wounds in the Vacuum-Assisted Closure (VAC) Group (81.8%) closed within 5 weeks, whereas only 60% of those in the conventional dressing group closed within 8 weeks [7]. Five patients in the conventional dressing group failed to heal within the duration of 8 weeks (56 days), resulting in treatment failure, whereas only one patient in the Vacuum-Assisted Closure (VAC) dressing group failed. Overall, Vacuum-Assisted Closure (VAC) dressing seems to be a novel method for dressing lower limb diabetic ulcers with better outcomes than conventional dressing.
Conclusion
In this study, it was found that the Vacuum-Assisted Closure (VAC) dressing was advantageous over conventional dressing for the dressing of lower limb diabetic ulcers in terms of the time taken for the formation of granulation tissue, the time taken for wound culture to be negative and long-term follow-up, and the duration of wound healing. Vacuum-Assisted Closure (VAC) dressing for chronic wounds or ulcers seems to be a promising option for treating conventional dressing, and the short-term results are good. However, compared with conventional dressings, VacuumAssisted Closure (VAC) dressings can cause a monetary burden on patients. Thus, based on our experience in this study, the use of a Vacuum Assisted Closure (VAC) dressing is suggested as a feasible technique for treating chronic ulcers, especially diabetic ulcers.
Author Contribution
Study conception and design: Piyush Ranjan
Acquisition of data: Piyush Ranjan, Rishika and Saptarshi Mondal
Analysis and interpretation of the data: Piyush Ranjan
Drafting of manuscript: Piyush Ranjan
Critical revision of manuscript: Rishika, Saptarshi Mondal
References
- Dsouza C, Diaz E, Rao S. A randomized controlled trial comparing low-cost vacuum assisted dressings and conventional dressing methods in the management of diabetic foot ulcers. Int Surg J. 2017;4:3858-3865.
- Nalini S, David G, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217-228.
[Crossref] [Google Scholar] [PubMed]
- Reiber GE, Vileikyte L, Boyko EJ, del AM, Smith DG, et al. Causal pathways for incident lower extremity ulcers in patients with diabetes from two settings. Diabetes Care. 1999;22:157-162.
[Crossref] [Google Scholar] [PubMed]
- Frykberg RG. Diabetic foot ulceration. The high risk foot in diabetic mellitus. 1990:151-195.
- Frykberg RG. Diabetic foot ulcers: current concepts. J Foot Ankle Surg. 1998;37:440-346.
[Crossref] [Google Scholar] [PubMed]
- Frykberg RG, Zgonis T, Armstrong DG, Driver VR, Giurini JM, et al. Diabetic foot disorders: a clinical practice guideline (2006 revision). J Foot Ankle Surg. 2006;45:S1-S66.
[Crossref] [Google Scholar] [PubMed]
- Lone AM, Zaroo MI, Laway BA, Pala NA, Bashir SA, et al. Vacuum-assisted closure versus conventional dressings in the management of diabetic foot ulcers: a prospective case–control study. Diabet Foot Ankle. 2014;5:23345.
[Crossref] [Google Scholar] [PubMed]
- Chariker ME, Jeter KF, Tintle TE, Bottsford JE. Effective management of incisional and cutaneous fistulae with closed suction wound drainage. Contemp Surg. 1989;34:59-63.
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38:563-576.
[Google Scholar] [PubMed]
- Morykwas MJ, Argenta LC. Non-surgical modalities to enhance healing and care of soft tissue wounds. J South Orthop Assoc. 1997;6:279-288.
[Google Scholar] [PubMed]
- Morykwas MJ, Argenta LC, Shelton-Brown EI. McGuirt Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg.1997;38:553-562.
[Crossref] [Google Scholar] [PubMed]
- Hasan MY, Teo R, Nather A. Negative-pressure wound therapy for management of diabetic foot wounds: a review of the mechanism of action, clinical applications, and recent developments. Diabet Foot Ankle. 2015;6:27618.
[Crossref] [Google Scholar] [PubMed]
- Kolsawala H, Gohil V, Saiyed A, Dhameliya A. A randomized comparative study of vacuum assisted dressing v/s conventional dressing in management of chronic wounds in diabetic patients. Eur J Mol Clin Med. 2022;9:834-842.
- Al-Mallah A, Al-Sayed A, Bayoumi A. Negative pressure wound therapy versus conventional dressing in treatment of diabetic foot wound. Egypt J Hosp Med. 2018;72:4054-4059.
- Riaz MU, Khan MU, Akbar A. Comparison of vacuum assisted closure versus normal saline dressing in healing diabetic wounds. Pak J Med Health Sci. 2010;4:308-313.
- Ali Z, Anjum A, Khurshid L, Ahad H, Maajid S, et al. Evaluation of low-cost custom made VAC therapy compared with conventional wound dressings in the treatment of non-healing lower limb ulcers in lower socio-economic group patients of Kashmir valley. J Orthop Surg Res. 2015;10:1-10.
[Crossref] [Google Scholar] [PubMed]
- Janugade HB, Chabbra RS, Das AG, Surushe A, Saygaonkar H. Outcomes of VAC versus conventional dressings in patients with lower limb ulcer. Int Surg J. 2018;5:1792-1796.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.